Highlights
I had a particularly rough time with chemotherapy, as I encountered some of the rarer side effects. Most testicular cancer patients have a much easier experience with chemotherapy. Nevertheless, this cancer diary will contain a lot of useful information, even for patients who aren't being treated with chemotherapy.
Age at diagnosis: 36 years old
- 05-01-2003: Testicular mass detected.
- 05-16-2003: Ultrasound confirms testicular cancer.
- 05-21-2003: Orchiectomy.
- 05-26-2003: Pathology identifies the cancer as pure seminoma.
- 05-30-2003: CT scan identifies three nodal masses, indicating stage III.
- 06-13-2003: Post-orchiectomy semen analysis normal, with sperm concentration of 45 million per ml, forward progression 67%, activity 2-2++, round cells 0-1 million/ml, and agglutination 0%.
- 06-17-2003: First day of first cycle of 3BEP chemotherapy.
- 06-23-2003 through 06-29-2003: Hospitalized for severe nausea and abdominal pain.
- 06-24-2003: ERCP and x-rays identify pancreatitis and gall stones.
- 06-25-2003: Gall bladder removed laparascopically.
- 07-02-2003: PET scan was inconclusive because the bone marrow responded very strongly to the neupogen, leading to the possibility of a false positive.
- 07-14-2003: First day of second cycle of 3BEP chemotherapy.
- 07-22-2003 through 07-24-2003: Hospitalized for severe nausea, severe abdominal pain and bone pain.
- 08-01-2003: Diabetes diagnosis, likely caused by pancreatitis and decadron.
- 08-05-2003: First day of third cycle of 3BEP chemotherapy.
- 08-07-2003 through 08-12-2003: Hospitalized in an attempt to control the nausea and abdominal pain before it occurs.
- 08-21-2003: Last day of chemotherapy.
- 09-09-2003: Second CT scan shows that the nodal mass adjacent to my heart has disappeared and the other two nodal masses have decreased in size. The larger of the two has shrunk from 3 cm to 1 cm.
- 10-08-2003: Second PET scan shows no evidence of FDG avid malignancy.
- 10-16-2003: Surveillance phase begins.
- 11-13-2003: CT scan shows possible metastases to the lower right lobe of the lung.
- 11-19-2003: PET scan followup to the CT scan shows no evidence of disease.
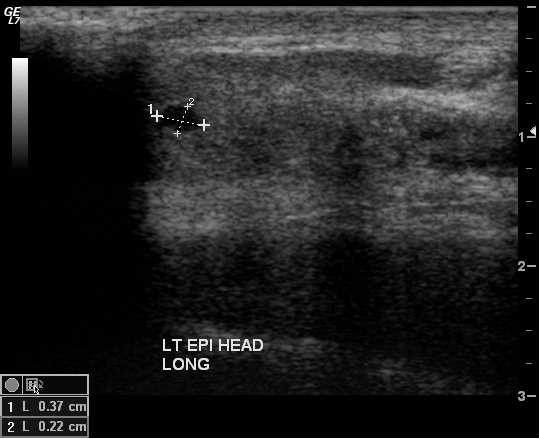
- 01-21-2004: Testicular Ultrasound shows contralateral testicle unchanged.
- 01-21-2004: Tumor markers are all normal.
- 01-21-2004: CT scan shows no sign of metastatic disease or disease progression.
- 03-23-2004: Tumor markers are all normal.
- 03-23-2004: CT scan shows no sign of metastatic disease.
- 07-06-2004: CT scan shows no sign of metastatic disease.
- 07-06-2004: Semi-annual ultrasound shows contralateral testicle unchanged.
- 07-16-2004: One year post-chemotherapy semen analysis subfertile, with sperm concentration of 16 million per ml, forward progression 69%, activity 2+-2++, round cells 0-1 million/ml, and agglutination 0%.
- 11-08-2004: Tumor markers are all normal.
- 11-08-2004: CT scan shows no sign of metastatic disease.
- 01-06-2005: Semi-annual ultrasound shows contralateral testicle unchanged.
- 03-14-2005: CT scan shows no sign of metastatic disease.
- 07-26-2005: Semi-annual ultrasound shows contralateral testicle unchanged.
- 09-19-2005: CT scan shows no sign of metastatic disease. Incidental findings of gynecomastia.
- 12-22-2005: Semi-annual ultrasound shows contralateral testicle unchanged.
- 02-13-2006: CT scan shows no sign of metastatic disease.
- 08-07-2006: Tumor markers are all normal.
- 08-07-2006: CT scan shows no sign of metastatic disease.
- 08-08-2006: Semi-annual ultrasound shows contralateral testicle unchanged.
- 12-21-2006: Tumor markers are all normal.
- 12-21-2006: CT scan shows no sign of metastatic disease. Possible nonfunctional neuroendocrine tumor of the pancreas. Same 1 cm mass was apparently present on my original staging CT scan, but missed by the radiologist.
- 1-4-2007: Abdominal MRI confirms the presence of a 1 cm mass at the tail of the pancreas. The MRI rules out adenocarcinoma of the pancreas, but cannot differentiate between neuroendocrine tumor of the pancreas and metastasis from the testicular cancer.
- 2-19-2007: Semi-annual ultrasound shows contralateral testicle unchanged.
- 2-19-2007: Total testosterone levels below normal, but free testosterone, FSH and LH all normal.
- 3-9-2007: PET-CT scan shows no sign of FDG avid malignancy.
- 5-14-2007: EUS-FNA biopsy of mass at tail of pancreas.
- 6-21-2007: Dedicated CT scan of the pancreas finds a second 1.5 cm mass in the body of the pancreas in addition to the 1.0 cm mass in the tail of the pancreas. Review of prior CT scans finds the second mass present as well and stable in size.
- 7-24-2007: Semi-annual ultrasound shows contralateral testicle unchanged.
- 7-26-2007: CT scan shows no sign of metastatic disease. Two pancreatic lesions are unchanged in size.
- 8-8-2007: Second EUS-FNA biopsy of mass at tail of pancreas.
- 7-24-2007: Semi-annual ultrasound shows contralateral testicle unchanged. Urinalysis shows glucosuria.
- 12-20-2007: CT scan shows no sign of metastatic disease. The tail lesion in the pancreas is unchanged in size. The radiologist did not remark on the body lesion. Tumor markers all normal.
- 1-25-2008: Semi-annual ultrasound shows contralateral testicle unchanged. Normal PSA. Total testosterone again deficient.
- 2-28-2008: Bone density test (DEXA) shows spinal cord density to be osteopenic. Left hip is normal.
- 7-21-2008: CT scan shows no sign of metastatic disease. The tail lesion in the pancreas is unchanged in size. The radiologist did not remark on the body lesion. Tumor markers all normal (including both testicular and pancreatic tumor markers).
- 7/30/08: Semi-annual ultrasound shows contralateral testicle unchanged. Urinalysis shows glucosuria.
Detailed Chronology
| May 1, 2003 (Thursday) |
I noticed some anomalies involving my right testicle
during my monthly testicular self-exam:
I wasn't in any pain. I spent a few hours doing some research on the web, and found only four possible causes of a testicular mass: epididymo-orchitis (infection), spermatocele (outpouching of tissue around the epididymis), hydrocele (fluid around the testicle), and testicular cancer. My symptoms were most consistent with the latter.
|
||||
| May 3, 2003 (Saturday) |
I told my wife about my suspicions, and that I'd be seeing the doctor
on Monday. The timing is rather bad, coming about two weeks after the
birth of my son. My wife still has severe back pain from the delivery,
and is confined more or less to the nursery until she
recovers. Currently, I'm waiting on her hand and foot, since she
can't shuffle more than 15 feet and can't go up and down stairs.
The
doctor prescribed anti-inflammatory drugs for her, so hopefully she'll
recover by the time we have to switch roles.
|
||||
| May 5, 2003 (Monday) |
My doctor confirmed the presence of a testicular mass. He also
threw in a prostate exam, finding that my prostate was normal. He had
me give urine and blood samples (to test for signs of infection) and
scheduled me for a testicular ultrasound on Friday, May 16.
My doctor demonstrated a reluctance to speculate about the diagnosis, beyond stating that it was a testicular mass. Strictly speaking, he should have assumed that it was testicular cancer until proven otherwise, and scheduled the ultrasound with greater urgency. He should have called various hospitals and labs until he found one that could conduct a testicular ultrasound the same day, instead of forcing me to wait two weeks. In hindsight I probably should have gone to the emergency room instead of my regular doctor. This would have yielded a much quicker diagnosis.
|
||||
| May 16, 2003 (Friday) |
By the time of my ultrasound, the testicular mass had doubled in size,
and was about the same size as a normal testicle.
The ultrasound is the exact same device they use for looking at a fetus in the womb. They use the same kind of goo too. I took a shower after getting home to get the goo off, since a wet paper towel at the hospital didn't do much good. During the ultrasound, the technician confirmed that the testicular mass was solid, meaning that it was a tumor. I asked for and received a copy of the ultrasound images, which turns out to have been a very smart move, as I was able to bring them with me when I saw a urologist. The official report on the ultrasound was not available until mid-morning on Monday, May 19.
|
||||
| May 19, 2003 (Monday) |
My doctor called with the results, confirming the presence of a solid
tumor. I asked him to fax me a copy of the ultrasound report. In
addition to the tumor, the report showed bilateral microlithiasis,
something my doctor forgot to mention.
I called and arranged for an appointment to see Dr. Musmanno, a urologist, the same day. Dr. Musmanno confirmed that it was testicular cancer, showing me on the ultrasounds where the tumor had taken over about three-quarters of the testicle. He also indicated that the fact that the tumor and the testicular mass showed varying densities was a potential sign of a non-seminoma. My urologist said that it was urgent to remove the cancerous tissue within the next 24-48 hours, and scheduled me for an orchiectomy at 9 am on Wednesday, May 21. I had a new version of my will notarized, along with a healthcare power of attorney and other documents. I had been working on a new will anyway, because of the birth of my son, but the diagnosis gave it a heightened sense of urgency.
|
||||
| May 20, 2003 (Tuesday) |
I went in to the hospital for pre-operative testing. They took blood
and urine samples, as well as a chest X-ray. Dr. Musmanno didn't try
scheduling me for a CT scan that day, since he didn't want to risk
delaying the orchiectomy.
|
||||
| May 21, 2003 (Wednesday) |
My orchiectomy was scheduled for first thing in the morning at West
Penn Hospital. My wife drove me there, since I would not be able to drive
for three weeks after the operation.
It's kind of interesting that the hospital has only one bathroom with a changing table, and it is too high for most women to use. So my wife changed my son on the floor in the ambulatory surgery waiting room. You'd think that a hospital would have changing tables in more of its bathrooms. After changing into the hospital gown (actually two gowns, one to cover the front and one to cover the rear), I got onto a gurney in a curtained waiting area. Various nurses and the anesthesiologist came to take my vitals, hook me up to an IV, and ask questions about allergies to medicines and anesthesia. They told me my chest X-rays were clear. Dr. Musmanno also came to see me before the operation. They gave me a sedative through the IV and wheeled me into the operating room, where they put me under with general anesthesia. During the orchiectomy they make a three-inch horizontal incision in the abdomen just below the belt line. They use it to remove not only the testicle but also some of the plumbing connected to it. This prevents the cancer from contaminating adjacent tissue, and also allows the pathologist to determine how much the cancer has spread. One thing doctors never seem to tell you before an operation (shouldn't this be part of informed consent?) is the fact that they will shave off any hair in the operative area. The pubic hair is very prickly as it grows back. I woke up in the recovery room with a big bandage on my abdomen and a pack of ice. Dr. Musmanno said the procedure went very well, and that the tumor appears to be a seminoma externally. Of course, we won't know for certain until we get the pathology report. After making sure I could still urinate, they discharged me at 3:15 pm with a prescription for painkillers (Oxycodone). For the next two days I had to keep ice on the incision and scrotum to keep the swelling down, changing the ice every 15-20 minutes. The painkillers weren't very effective, only taking the pain down a notch or two. The bags of ice were much more effective. Since the ice was rather cold, wrapping it in a paper towel helped. The pain and the painkillers interfered with my ability to concentrate. One thing they should include in the discharge instructions is to avoid laughing. Laughing is excruciatingly painful. My wife gave me a large container of Poppycock, not realizing the humor inherent in the name. My prescribed pain medication ran out on May 24, 2003. My doctor told me to take extra strength Tylenol when I ran out of the other pain medication. But the Tylenol was completely ineffective at controlling the pain. His other suggestion was to put a bag of ice wrapped over the incision area. This worked, controlling both the pain and the swelling. A bag of frozen peas or corn wrapped in a paper towel worked best, since it could be easily molded to fit the abdomen. Visually, the scrotum looks much like it did before, only with a little less stuffing. My underwear still fits well.
|
||||
| May 26, 2003 (Monday) |
The pathology report found that the tumor was a high grade
malignant seminoma with spermatic cord invasion. The tumor
involved the testicle, extending into the epididymis and
up into the spermatic cord. (The largest tumor dimension was 3.5
cm. The dimensions of the tumor in the testicle was 3.5 x 3.4 x 3.0
cm. In the epididymis the dimensions were 3.0 x 1.7 x 2.0 cm. In the
spermatic cord, the dimensions were 1.5 x 1.4 x 1.4 cm.) But it appears to not have
gone beyond the spermatic cord, as the spermatic cord
margin was free of neoplasm. There was also no sign of
neoplasm in the blood vessels or lymph vessels next to
the tumor, nor in the tunica vaginalis (the outer layer
surrounding the testicle).
|
||||
| May 27, 2003 (Tuesday) |
I find it kind of amazing that people expect me to be embarrassed or
emotional about the cancer or the orchiectomy. Yes, I have cancer, and
yes, I now have only one testicle, and yes, there's a good chance I
may die. So what? Will running around like a
headless chicken cure the cancer? Worrying won't accomplish
anything. Educating myself about testicular cancer
and treatment options is the best use of my time. I prefer to be
pragmatic and rational about it.
Incidentally, the bandages around the incision itch a lot, as does all the hair growing back. The end of each hair is like a little pin, pricking my skin. Changing the bandages helped a little. After the steri-strips from the orchiectomy came off, I tried using a half dozen regular bandaids, since there was a small amount of bleeding every time the scabs cracked. This didn't work well. What worked much better is an adhesive pad, like the 3M Medipore +Pad (brand name "Nexcare"). The bandage part is 1" x 2-3/8", which is too short to cover the full length of the incision. But if you cut off the end of one pad and overlap it with the end of another, it works well.
|
||||
| May 29, 2003 (Thursday) |
I called my urologist because I felt what I thought
was new growth, and because I had lost six pounds since the day after
the operation. Dr. Musmanno wasn't available, so I saw Dr. Sholder
instead. Like Dr. Musmanno, Dr. Sholder has very good bedside manner.
Dr. Sholder had me come in for an exam. The "new growth" was
actually the sutures at the bottom of the scrotum, along with normal
fluid buildup. The weight loss was also normal after an operation. He
said that cancer patients often become concerned about every lump they
feel, and that I should not hesitate to call Dr. Musmanno if I have any
concerns.
|
||||
| May 30, 2003 (Friday) |
I went to the hospital for CT scans of my pelvis, abdomen, and chest,
with and without contrast die. As with the ultrasounds, I asked for
and received a copy of the CT scans.
They made me drink two quarts of
a milky white barium sulfate solution. The berry flavor barely masks
the chemical taste, and does nothing about the texture. I drank so
much of the stuff that I was full to the gills. They also hooked me up
to an IV for intravenous contrast die (120 cc of Optiray 320). The nurse jabbed the needle
through the nerve on the way to the vein, causing intense extreme pain
to my thumb and index finger. The pain went away after about 5
minutes. During the CT scan itself I felt very hot, the way a piece of
food must feel when it is being nuked in a microwave. About an hour
after the CT scan I had massive diarrhea, with a considerable amount
of liquid coming out all at once. Luckily I was near a bathroom at the
time.
I looked at the CT scans afterward. Although I could identify various organs (heart, lungs, intestines, spinal cord, kidneys), I was unable to determine whether they were normal or abnormal. So I will just have to wait until my appointment with Dr. Musmanno on Monday.
|
||||
| June 2, 2003 (Monday) |
I scheduled a dentist appointment for the morning before my
appointment with Dr. Musmanno. This was partly because I had heard
that it is a good idea to have complete dental work before starting
chemotherapy, as chemotherapy patients are more prone to mouth sores,
bleeding and infection. Also, when they intubated me during the
operation, they chipped some bonding agent off of one of my lower teeth.
|
||||
| June 2, 2003 (Monday) |
I saw Dr. Musmanno for a follow-up appointment to examine the incision
area and my recovery, and to review the CT scans and talk about a
treatment plan.
The incision is healing nicely. There's a raised ridge of tissue under the incision -- the so-called "healing ridge". Aside from that, the swelling has gone down. Dr. Musmanno says that I can drive a car again. The radiologist's report said that the CT scan found three tumors in lymph nodes, two in the chest and one in the abdomen:
|
||||
| June 2, 2003 (Monday) |
Dr. Barsouk reviewed my records, took a look
at the CT scans, and pulled in a radiologist consult on the CT
scans. He confirmed that it is stage III testicular cancer. My
chemotherapy is scheduled to begin on Monday, June 16. The only
variable at this point is whether it will be 3 cycles of BEP
chemotherapy (BEP = Bleomycin, Etoposide, and cisPlatin) or 4 cycles
of EP chemotherapy. 4EP is thought to be about as effective as 3BEP
for good risk patients, but with less toxicity. Dr. Barsouk is leaning
toward 4EP, but we won't make a decision until June 16. I will read
everything I can find concerning treatment of stage III testicular cancer.
He's scheduled a pulmonary function test in case I decide to go with 3BEP.
I will also have a PET scan and do sperm banking.
|
||||
| June 3, 2003 (Tuesday) |
First sperm banking appointment. After I
filled out several forms and they
drew blood for viral testing, they showed me to a collection room. No
videos, just a few magazines.
Very clinical atmosphere, with
disposable antiseptic pads for the chair and the same type of
collection bottle they use for urine samples. The room must have been
a walk-in closet at some point, because there were still boxes of
stationery supplies in one corner. The task isn't as easy as it might
seem, because one must catch the ejaculate in the collection
bottle. You try walking, talking, patting your head and rubbing
your tummy at the same time. It also doesn't help that the hair has
started growing back like hundreds of tiny needles (they shave you for
the orchiectomy). I called later and they
told me the sample produced 4 vials. Since the goal is 18 vials, I
will need the remaining 4 appointments. The appointments are separated
by at least 2 and no more than 5 days for optimum sperm quality.
|
||||
| June 3, 2003 (Tuesday) |
My urologist is calling Indiana University to
get a consultation on my case. Stage III Seminoma is actually quite
rare, and they should have more experience treating this type of
testicular cancer. He believes that it might be beneficial
for me to undergo radiation therapy in addition to chemotherapy. He
will also talk to my oncologist about whether a head CT scan is
necessary.
|
||||
| June 4, 2003 (Wednesday) |
My urologist says that the folks at Indiana
University do not recommend radiation therapy in conjunction with
chemotherapy. They only typically recommend it for stage II
cases. They say that either 4EP or 3BEP chemotherapy is recommended,
and that I might want to lean toward 4EP because of the lower
toxicity. He also said that unless I'm experiencing neurological
changes, there's no need for a head CT scan, but that he would
schedule it if I need it for peace of mind. (Very punny!)
My son has been smiling for weeks, but this is the first time he smiled when I wasn't holding him, so I could take his picture.
|
||||
| June 4, 2003 (Wednesday) |
Some colleagues asked for my favorite
charity. It is the
Center for Excellence in Education,
a tax exempt 501(c)3 education foundation. Donation information
can be found on the
Get Involved
page.
|
||||
| June 5, 2003 (Thursday) |
Called 1-800-4-CANCER (1-800-422-6237) and
ordered some of the American Cancer Society's free booklets on cancer
treatment.
|
||||
| June 5, 2003 (Thursday) |
I sent email to Dr. Einhorn at Indiana
University with questions about the relative effectiveness and
toxicity of 4EP vs 3BEP. 3BEP is the standard treatment, but 4EP is
offered as an alternative to avoid the toxic effects of
Bleomycin. There is a study by Bajorin, Bosl et al that suggests that
4EP is as effective as 3BEP with reduced toxicity. But I could find no
independent study that confirmed this. In fact, I found three studies
that shed doubt on this result. Dr. Einhorn responded right away that
Culine had presented a paper this week at ASCO showing a cure rate of
96% for 3BEP and 92% for 4EP, with 5 3BEP deaths and 10 4EP deaths. He
also noted that he feels that 4EP is far more toxic than 3BEP because
of "cumulative platinum related neurotoxicity, anorexia, nausea, and
ototoxicity as well as the small risk of leukemia with etoposide at
higher total dosage". He also noted that they almost never see
patients with Raynaud's Phenomenon and that it is not certain that
Bleomycin is the culprit. I was originally leaning toward 3BEP and
this reinforces that inclination. Unless the pulmonary function
testing raises an issue or my doctors can convince me otherwise, I'm
going to go with 3BEP.
|
||||
| June 5, 2003 (Thursday) |
My beta-HCG levels are 37 mIU/ML
as of June 2, 2003, down from 156 mIU/ML on May 20, 2003. The latter
was before the orchiectomy and the former after. The half-life of
beta-HCG is 24 to 36 hours, meaning that beta-HCG should return
to normal about a week after surgery. Normal levels are less than 5
mIU/ML. The fact that the levels are dropping is a good sign. However,
the fact that they are still above normal is probably an indication
that the other three tumors are still producing beta-HCG. This is good
news, because it means we can use beta-HCG levels as an indication of
the cancer's response to treatment.
Beta-HCG levels are also elevated during pregnancy, typically reaching 10-50 mIU/ML in the week following conception, and peaking at 288,000 mIU/ML about two months after conception. Home pregnancy tests typically signal a result when beta HCG levels are at least 25 mIU/ML (e.g., the ept test requires 40 mIU/ML, Clearblue Easy 25 mIU/ML, and Confirm 25 mIU/ML). Since my beta-HCG levels were 37 mIU/ML, I was curious whether they were high enough to be measured by one of those home pregnancy tests. Turns out that my beta-HCG levels are just barely enough to trigger the ept test, as is demonstrated by the following photograph. Pretty funny, eh?
|
||||
| June 9, 2003 (Monday) |
The cryopreservation report shows a sperm concentration of 19
million/ml, forward progression of 74%, activity of 2++, round cells
of 0-1 million/ml, and agglutination of 0%, all normal. A
small sample was frozen and thawed, with a post-thaw density of 4
million/ml, forward progression of 56%, activity of 1-2++, and total
motile cells per vial, based on 0.2 ml volume, of 448,000. These are
good results, indicating that the cryopreservation should be
successful. The viral testing came back all negative, as expected.
They've frozen a total of 10 vials for me so far, leaving 8 to
go. I'll probably fall short by 1 or 2 vials due to the time
constraints, but that is ok.
|
||||
| June 9, 2003 (Monday) |
Today I had an appointment with my regular
physician, partly for a routine physical and partly to bring him up to
date. I've lost 8 pounds since my last appointment. Aside from the
cancer, I'm rather healthy, which bodes well for my ability to handle
the chemotherapy. He also signed the form to get me a temporary
disabled parking placard for the duration of the chemotherapy.
The dentist appointment didn't go as well. A cavity was found on the face of one of my wisdom teeth, and the decay went all the way to the nerve. Since root canals are not normally performed on wisdom teeth, however, the only option is a simple extraction. (Luckily, the tooth is not impacted.) Unfortunately, an extraction would require at least 21 days to heal (actually, more like 6 months to fully heal, but 21 days is the minimum), which would interfere with the chemotherapy schedule. Since the chemotherapy cannot be delayed, the extraction will simply have to wait until the chemotherapy is complete and my platelet and white blood cell counts return to normal. In the meantime I have a temporary filling and some Tylenol for the pain. (Ibuprofen and aspirin are prohibited because they are blood thinners.) I've been reading about chemotherapy and diet. The good news is they recommend eating ice cream and drinking soda to keep hydrated and avoid constipation. The bad news is chemotherapy will probably make everything taste metallic.
|
||||
| June 10, 2003 (Tuesday) |
Because Bleomycin can cause pulmonary fibrosis and impair lung
function, a prerequisite for 3BEP chemotherapy is to check lung
function. This is partly to make sure my lung function isn't already
impaired, and partly to establish a baseline for later comparison. So
today I went to the hospital for pulmonary function
testing. This involves breathing into a tube while a nose clip closes
off the nasal passages. The tests measured lung capacity, diffusion
rates and flow, and required me to breathe in various ways, such as:
breathing normally, holding my breath,
pushing out as much air as possible as quickly as possible, panting, and
breathing as though I had just run a marathon (3/4 breathes in and out
very rapidly). It was actually kind of fun, except for when I
accidentally swallowed with the nose clip on. (That made my ears want
to pop in a kind of reverse valsalva maneuver.)
My results were all good, with several above average. My hemoglobin
was 15.9.
|
||||
| June 11, 2003 (Wednesday) |
The PET scan was supposed to be today, but it's been cancelled because
it needs to be "authorized". Apparently, use of a PET scan is not yet
common with testicular cancer. My oncologist ordered the PET scan
because he wanted to see if the tumors in my chest were metabolically
active. If they weren't, then perhaps I'm stage II instead of stage
III. If they were, then a follow-up PET scan after treatment could be
used to determine whether there was still active cancer in the
nodes. (Apparently chemotherapy with seminomas has a tendency to leave
fibrotic tissue behind, making it difficult to determine with a CT
scan whether the cancer has responded to treatment or not.)
|
||||
| June 12, 2003 (Thursday) |
I went to the hospital today to have my head examined, to make sure
there are no tumors in the brain. This time there
was no barium sulfate solution to drink, since it was just a head CT
scan, but they did give me contrast dye through an IV. The IV was in
my arm, instead of my wrist, so the nurse didn't hit the nerve. The head CT is
fascinating. I can see my eyes, nasal passages, and the folds in the
brain. Again, I don't know what's normal and what's not, so I will
have to wait for the radiologist's report. But at least there's no
sign of a little alien homunculus pulling the strings.
After the CT scan I went down to pathology to pick up a copy of the slides for a second opinion at the Indiana University Medical Center. The pathologist, Dr. Lynch, gave me a guided tour of my pathology slides. He said that this was the first time he's shown a patient his pathology slides. It was fascinating. First he showed me normal testicular tissue. I saw the seminiferous tubules lined with Sertoli cells and with small round germ cells in the center and some spermatids (immature sperm). He also showed me a few Leydig cells, which produce testosterone. Then he showed me the cancerous tissue, which was completely filled with germ cells. He showed me examples from the testicle, the epididymis, and the spermatic cord. Except for occasional lymphocytes responding to the cancer, it was uniformly germ cells. That's a pretty clear indication of a seminoma. I'm still going to send the slides on to Indiana University, just to be sure. Seeing the pathology slides was helpful in another way. Consciously I always knew that cancer is the body's own cells multiplying unchecked, but unconsciously I had a misconception that it was something external invading the body. Seeing the slides make it clear on all levels that this was my own germ cells multiplying ad infinitum. Of course, the cause is probably still something external, such as DES, other hormones (synthetic or otherwise), pesticides or environmental pollutants. But the mechanism of the disease is my own cells multiplying unchecked and spreading. A friend in Chicago sent me a box full of Caffeine-free Dr. Pepper, since you can't get it here in Pittsburgh.
|
||||
| June 13, 2003 (Friday) |
My last sperm banking appointment was today. The five appointments
yielded a total of 18 vials. On average, six vials is enough to
achieve a single pregnancy with IVF, since IVF normally has a 15% to
18% success rate. The total
cost, including viral testing, processing of the samples
and storage, comes to $2,180.
My oncologist called around noon to say that he presented my case to the tumor board and they felt that even though I'm stage III, I'm a candidate for radiation therapy because my tumors are non-bulky and seminoma. He said that the small size of the tumors in my chest means I'm borderline between stage II and stage III, and seminoma is very susceptible to radiation therapy. If radiation therapy works, I could avoid some of the toxicity and negative side effects associated with chemotherapy. If radiation therapy failed, I could do chemotherapy later. I have a lot of misgivings about this, especially the last minute nature of the change. I've agreed to see a radiation oncologist on Monday, after being assured that if I decide to go with chemotherapy, I could still begin chemo on Monday, just a few hours delayed. But unless she's very convincing, I'm going to go with 3BEP chemotherapy. Everything I've read indicates that chemotherapy is the preferred initial treatment in my situation. This is definitely a roller coaster, and I'm going to have to cram this weekend to read everything I can about radiation therapy. I've been focusing exclusively on the risks and benefits of different forms of chemotherapy during the past few weeks. I ignored radiation therapy in part because I thought I wasn't a good candidate for it, and in part because I had read that chemotherapy is often more effective. Some of my concerns include the following:
I do not want to play with fire just for a chance of possibly avoiding the greater toxicity of chemotherapy. It's quite clear to me that I need systemic treatment, since the cancer has clearly spread and is not contained to a specific area of the body. If by any chance she convinces me to consider radiation therapy, my agreement will be contingent on my having another CT scan on Monday to check on the state of the tumors. If they can't get me a CT scan on Monday, I'm going with chemotherapy. If the CT scan shows that the tumors have grown or spread, I'm going with chemotherapy.
|
||||
| June 15, 2003 (Sunday) |
I am not looking forward to any kind of port or catheter. The idea of
a tube snaking through my veins into my heart gives me the
willies. I've got good veins, and don't have a problem with needle
pricks (so long as they don't pierce a nerve), so perhaps they won't
need a vein access device with me.
I've noticed in myself a tendency to indulge a little more since the cancer diagnosis. But it seems to be limited to things that I need, not things that I want. If I need something and would have hesitated before because of cost, I'm more likely to buy it now. But I still show self-restraint for expensive items that I don't really need, like the Segway HT.
|
||||
| June 16, 2003 (Monday) |
The radiation oncologist said that they have doubts whether
the tumor near my heart is cancer or not, and this would make a
difference in whether I'm stage II or stage III. However, she
recommends chemotherapy in my case, because radiation therapy risks
undertreating me and because they would also need to subject part of my
heart and lungs to radiation. My medical oncologist concurred, saying
that he just wanted to present me with all the options. This gives me
greater confidence in my oncologist.
My schedule will be cisPlatin and Etoposide every day of the first week of each cycle, running from about 9 am to about 3 pm, and Bleomycin the second day of every week for all 9 weeks. I'm not sure how long the Bleomycin will take (i.e., whether it is also an all-day affair). I'm also not sure whether they will reset me to a Monday-Friday schedule with the second cycle. Unfortunately, it was too late in the day to start 3BEP, so I will start tomorrow (Tuesday), at 8:30 am. My head CT scan came back clear, so there are no brain tumors. They did not that I have chronic left maxillary sinusitis. My oncologist still wants me to have a PET scan, and is fighting with my insurance company to get it approved. In particular, he wants to know whether the mass near my heart is metabolically active. He says that if the PET scan is to happen, it must happen no later than next week. If my insurance doesn't cover it, it will cost me approximately $4,000. Hopefully they'll cover it. The good news is my insurance company has precertified the chemotherapy, so there shouldn't be any problems with that. While I was at the pharmacy to pick up a prescription for antibiotics (for folliculitis, nothing to do with the cancer, although my oncologist likes the idea of my taking them while on chemo), Eckerd told me that my insurance has me listed with the wrong date of birth. After a half dozen calls to the insurance company, the insurance company confirmed that they have me listed with the correct date of birth. The insurance company also said that they don't show any transactions from Eckerd for me today. So it looks like Eckerd is billing the wrong insurance company and/or the wrong individual. I've lost a total of 11 pounds since the day after the orchiectomy. That's enough that I'm in the last notch in my belt, and my pants still feel a little loose. I'll soon have to switch to another belt. I'll probably have to go shopping for new clothes when this is all over (i.e., Retail Therapy). So right now I feel pretty good, since I'm lighter than I've been in several years. Of course, I haven't started chemotherapy yet. I'm told that the chemotherapy starts affecting you after a few days, and really hits you in the second week. I mentioned to my doctor that I've suffered from high pitch hearing loss and tinnitus since I was a child, due to childhood ear infections. Since these can also be side effects of chemotherapy, I won't necessarily be able to tell whether I'm getting it because of the chemotherapy. It might be a good idea for me to get a hearing test after the chemotherapy is over, to see whether there was an effect.
|
||||
| June 16, 2003 (Monday) |
I am not worried about the cancer, nor do I fear it. I'm not the sort
to worry about much of anything. If something is beyond my control, I
don't waste time worrying about it, because nothing I can do can
affect it. If I can do something about it, I take action, rather than
waste time worrying about it. When I first suspected that I might have
cancer, I started reading everything I could find on the topic. I've
absorbed a considerable amount of material. I understand what will
happen and what might happen (and also what won't happen). So even if
the future is indeterminate, it is still well-defined. Knowledge is
the antidote to fear.
If I die, I die. I will have done everything I can to avoid that possibility, and I have taken steps to provide for my wife and son in case I do die. But other than that, I'm not going to waste time dwelling on the possibility. I do not have any regrets. I am aware that having a history of cancer is going to make it more difficult to get health and life insurance in the future. It may also affect my employability, regardless of any protections provided by the Americans with Disabilities Act. But there's nothing I can do about it. It it becomes an issue, I'll deal with it then. In some ways, cancer will actually be good for me. I'm about 45 pounds overweight, so I'll end up healthier in some ways after the treatment is complete. My wife does worry, but that's part of the job description. It helps that my newborn son keeps her busy much of the time, distracting her. He grows every day, so there's always something new. Today he was awake during our daily walk, turning his head to look at the scenery. I do feel some anger. I did not cause the cancer and it is disrupting my life. I do not have any of the risk factors other than age. I want to know who or what caused the cancer. I've read dozens of papers about statistics relating to testicular cancer and dozens of papers about endocrine disrupting chemicals like diethylstilbestrol (DES), DDT, and estradiol. I'm amazed that such chemicals are approved for use in agriculture, including several known carcinogens. Several of these chemicals are fat soluble, meaning that lifetime exposure could have a cumulative effect. The use of such chemicals is reckless, irresponsible, and just plain stupid. If I can prove a connection, I will take appropriate legal action to correct this situation. I do find amusing thoughts popping into my head, such as:
My aunt sent me a copy of a 40-page essay she wrote 12 years after she was diagnosed with breast cancer. It talks about the emotional reaction to cancer and feelings. She talks about worrying that the cancer might recur, about the cost of cancer care, and about feelings of abandonment. She should probably publish it as a book, as there are no existing books that address this topic.
|
||||
| June 17, 2003 (Tuesday) |
Today was my first day of chemotherapy. I arrived at 8 am, and they
had me hooked up to an IV for hydration by 8:30 am.
Before they started the hydration, the nurse took some blood through the IV for testing. I suggested that they also test my beta-HCG levels, since they have only two data points for me: the day before the orchiectomy, and 10 days later. The latter was two weeks ago, so beta-HCG levels now would tell them whether the levels continued to decay or started back up. Since beta-HCG levels are my only tumor marker, it's a good idea to have them checked right before each chemotherapy cycle. (My chart says CBC, platelet, LDH, total bilirubin prior to each cycle, but does not make any reference to beta-HCG.) The doctor agreed. She took the blood in a syringe, and transfered it to each test tube afterward. The side effects were manageable, although I'm aware that they will likely get worse. Also, I only got etoposide and cisplatin today; I won't get bleomycin until tomorrow. They gave me Zofran in the IV, and a prescription for use at home, so I didn't feel any nausea. The nurse who inserted my IV was amazing. I hardly felt anything at all. They use a special type of IV that removes the needle after insertion, leaving a thin tube behind, since the aluminum in standard needles reacts with cisplatin. After the IV was started, I could feel the cool drip of the IV fluid. First they used the IV to hydrate me for several hours. This meant I needed to pee every 30-60 minutes. The first time the nurse unhooked me from the IV, but the other times I just pushed the IV tree with me to the bathroom. Next I was given Zofran to prevent nausea. The main side effect of this was it made me a little drowsy for 15-30 minutes. It also gave me a light dullness (similar to what happens when I take migraine medication) and a stiff neck. Then I was given etoposide followed by cisplatin. They gave me an information packet about Neulasta (a successor drug to Neupogen). They will give it to me next week to increase my white blood cell counts. This helps fight infection. The information packet came with a free digital thermometer, since I'm supposed to take my temperature every evening. After getting home, my main side effects appear to be some fatigue, feeling warmer, and a metallic taste in my mouth (presumably from the cisplatin). Creme Savers hard candy seems to help with the taste. Also, my sinuses feel full, almost like I'm about to get a sinus headache, but not quite. My chemotherapy regimen is as follows:
Initially I'm starting a day late, since I started on a Tuesday. They will reset me to a Monday-Friday schedule on the second cycle. Wednesday June 25, 2003, I will have a PET scan in addition to the Bleomycin. They only do PET scans on Wednesdays. It still isn't clear whether the insurance company will pay for it, but hopefully they will. This morning I had lost another pound, even though I ate a big dinner (stuffed chicked breast). Also, I had a nosebleed after waking up, which manifested itself as congestion in the left nostril, resulting in four bloody tissues. I've been having them off and on for a few years, presumably due to allergies and sinusitis, and always in the left nostril.
The day itself was rather boring. There were two other chemotherapy patients for a short while (their chemotherapy did not require hydration). Other than that I was by myself. The TV gets local channels only and generates a high pitched whine while it is warming up, but they're working on getting cable and a new TV. I watched it for a little while, but Dr. Phil is insipid and inane, and the soap operas are even worse. I spent the rest of the time reading two technical journals, reading 30 pages from a science fiction book I brought with me, and folding an origami robin and a dragon. Tomorrow I will bring a laptop with me and get some work done. I can see why cancer patients describe getting chemotherapy as having paint remover poured into your veins. Chemotherapy is, after all, a derivative of chemical weapons like mustard gas. Doctors treating soldiers exposed to mustard gas noticed in 1942 that mustard gas affected rapidly dividing cells, suggesting that it might be an effective agent against cancer. They subsequently found that lymphoma patients given it by injection showed some improvement. Many modern chemotherapy drugs (alkylating agents) are descendants of mustard gas, albeit less toxic. (It doesn't help to cure the cancer if you kill the patient in the process.) So in some sense good arose from evil, in that a weapon of war lead to the development of a cure for cancer.
|
||||
| June 18, 2003 (Wednesday) |
When I woke up this morning, the Zofran had started to wear off. I
guess it does make a weird kind of sense to have morning sickness:
I shaved my arms, to make the medical tape stick better and avoid the pain of hairs being removed with the tape. Today the nurse put the IV in the forearm of my left arm instead of the inside elbow of my right arm. It didn't hurt going it, but later hurt a little, probably because it was close to the nerve. Using the forearm made it easier to type (I brought a laptop with me, so I could do some offline work).
Today I had Bleomycin. I did not have an immediate reaction. Bleomycin is known to cause fever and chills about four hours after administration. The oncology nurse told me to take two Tylenol if this happens and to call them if it is severe. Curiously, I didn't have much of a metallic taste today from the cisplatin. I did use many Cream Savers and lemon hard candy, so maybe that helped. All in all, my side effects today weren't as severe as yesterday. All I really have is mild fatigue. I did get a sore throat later in the evening, but it was rather mild and didn't last long. I have noticed a greater tendency for valid word spelling errors in my writing (i.e., its/it's, effects/affects, die/dye, have/has and so on). I wonder if this is somehow related to the chemo (i.e., fatigue), or just a coincidence. This morning my weight went up by two pounds. Three sandwiches for lunch and a big dinner, plus some fluid retention from the IV probably was responsible. I'll see what happens tomorrow. I finished my initial collection of cancer jokes. Some of them are quite funny.
|
||||
| June 19, 2003 (Thursday) |
Normally I only sleep 3-4 hours a night. However, ever since the
operation, I've been sleeping 8 hours a night. Last night was an
exception, where I again slept only 4 hours. I felt refreshed when I
woke up, so I wasn't concerned. I mentioned it to one of the nurses,
and she said that one of the drugs they gave me yesterday does that.
I was somewhat nauseous when I woke up, and that continued throughout the day. I did eat lunch, albeit around 2 pm, and was able to keep it down. The nausea was in the back of my throat, not in my stomach. I got my beta-HCG results from Tuesday, and they were 18 mIU/ml, about half what they were after the orchiectomy. It's nice that they're heading in the right direction. (At this level, however, I'll no longer be able to trigger a home pregnancy test.) At least it's a sign that Junior is starting to shrink. My oncology nurse likes to wear Sponge-Bob shirts. Today, when she removed the IV at the end of the day, she gave me a Sponge-Bob bandaid to cover the hole. One of the other nurses saw it and said "Annette's marking her patients again". I noticed that they gave me some Mannitol (25% 50 ml) and asked what it was for. My nurse said it is to make sure I pee, so that the drugs continue to be excreted from my system. I don't see how I could avoid peeing, given the amount of fluids I'm getting. Like the past two times I got the Zofran, I was drowsy and unable to concentrate for about 15-30 minutes after getting the last of it. I couldn't even focus enough to read. Most of the other patients aren't there for as long as me, so there are constantly changing faces every day. Today they were more talkative and engaging, so I shared my son's picture with them. (Most of the other patients are much older than me.) Since some of their caregivers have college-age children, I talked with them about college admissions and financial aid. I've also been using a small laptop to work on content for a new web site that will be of interest to the financial aid community. (I don't have net access while in the hospital, so I have to focus on offline work.) I have part of my schedule for next week, and will receive the rest of it on Friday. I will also be at the hospital on Saturday to receive my fifth day of chemotherapy. Since the oncologist's office is closed on Saturday, I will be receiving my chemotherapy in the hospital's short-stay wing. My nieces sent me a homemade get well card and a present. The card said "Hair ... More trouble than it's worth!" and the present was a plush bald eagle with a note "The bald eagle soars above all others!". They put a lot of thought into it, and it brought a smile to my face. The nausea continued throughout the evening, although it got a little better after I took a Zofran. Burping helped. Taking a bath didn't.
|
||||
| June 20, 2003 (Friday) |
Today was by far the worst day so far. Not only did I have severe
nausea all day, but I had a complete loss of appetite. My pee smelled
really bad. My ears started hurting in the afternoon, and my
tinnitus got worse. My nurse noticed that I had some bruises on my
arms, so my platelet levels must be reduced. I lost two pounds since
this morning. My skin felt like it was burning, but I did not have a
temperature. I also felt chilled at the same time, despite the
temperature in the room being set at 72 degrees. (I'm the sort of guy
who can normally go out and shovel snow in short sleeves in the middle of
winter and not feel cold. I also like to keep the house around 65
degrees, since I can easily get overheated. So for me to feel cold is
unusual.) I also had the usual
fatigue. As soon as I got home I went to bed, but couldn't sleep. I
was able to eat (and keep down) half a serving of macaroni, some
chocolate milk and some raisins.
I think my hair is starting to fall out. I normally shed a little chest hair now and then, but it seems to be increasing. I would not be surprised if it doesn't start coming out in bigger quantities over the next week or two, and if I start losing head hair as well. (When folks hear about chemotherapy patients losing their hair, they often don't realize that this means ALL hair, including body hair.) The only good news is tomorrow is the last day of main chemotherapy for the first cycle. I still have Bleomycin on Wednesdays for the next two weeks, and a Neulasta injection on Monday, but my next five-day course of chemotherapy isn't until July 7-11. I started keeping track of the costs associated with treatment. US Airways did agree to extend the exchange period for my cancelled flight to Chicago for one year, and will be mailing me a voucher for that trip.
|
||||
| June 21, 2003 (Saturday) |
Today was the fifth day of chemotherapy. Since my oncologist's office
was closed today, I received the chemotherapy in the hospital's
Medical Short Stay wing. I was nauseous all day, and it took all my
concrentration to avoid throwing up. But when the nurse
gave me the decadron as a shot instead of a slow drip, it made me very
hot and caused me to vomit up the lunch (salisbury steak, carrots,
mashed potatoes, chicken noodle soup and greaps). Vomiting doesn't
make you feel any better. My nausea was so bad
that they nurse had questions about whether they should discharge
me. Instead, she called my oncologist and gave me another drug for
nausea. This worked, but made me incredibly drowsy and completely
wiped me out.
In addition, my original IV was hurting during the hydration, so before they started the chemotherapy, they switched me to a fresh IV in my other arm. I was in such bad shape all day that I couldn't do anything, not even read. The nurse is recommending that I eat only clear liquids for the next few days. At least my blood counts all seem to still be within the normal range, although they've dropped somewhat.
|
||||
| June 22, 2003 (Sunday) |
This morning I woke up at 4 am because of the ringing in my ears and
couldn't fall back asleep. I took a Zofran, Decadron and antibiotic
with a little food at 6 am. That got rid of most of the nausea, but
there was still a background undercurrent of nausea I couldn't get rid
of. Sitting, standing, and lying in bed were all the same -- no
relief. Also, I think the burning sensation on my skin is peripheral
neuropathy. It affects the pinky and ring finger on each hand, the
back of the index finger and thumb, and runs up the outside of each
arm. I can still type, but it feels like I have a permanent case of
frostbite. My feet also feel like they want to go to sleep. I feel weak all
over and am popping Tums to keep the Decadron heartburn at bay.
I can no longer hold my son because my breath and sweat are now toxic due to the chemotherapy.
|
||||
| June 23, 2003 - June 29, 2003 |
I was hospitalized from Monday afternoon through
Sunday afternoon.
When I saw my oncologist on Monday, I was complaining of severe abdominal pain that had started Saturday evening after my chemotherapy and intensified throughout the weekend. A blood test showed signs of a possible problem, so he had me admitted to the hospital that afternoon as a precaution. I underwent multiple blood tests, X-rays, and an ERCP (Endoscopic Retrograde Cholangio-Pancreatography) because they suspected an inflamed pancreas. During an ERCP they put you under with general anesthesia and send a tiny camera down your throat to examine the pancreas, gallbladder and duodenum. The camera has attachments for making certain repairs (e.g., an inflatable ballon and a cauterizer) so they can fix certain problems while they're diagnosing the condition. In my case they found that I had acute pancreatitis and gall stones. They believe that the pancreatitis was caused by the chemotherapy and not by the gall stones. But they were concerned that the gall stones could potentially reinflame the pancreas so they recommended removing the gall bladder now, while my counts were still good. So on Wednesday I underwent laprascopic surgery to remove my gall bladder. During this procedure they go in through the belly button and two small holes in the chest and conduct the surgery in a minimally invasive manner. I've had a mildly herniated belly button for the past three years, so they fixed that at the same time. I was then on only IV fluids (nothing by mouth) for several days to allow the pancreas to recover. They also kept me in the hospital because I became extremely neutropenic (my white blood cell counts had plummeted after the surgery). Then, when they restarted me on food, starting with a liquid-only diet (juice, jello, beef or chicken broth), my digestive system had trouble restarting. I was having extreme diarrhea every 15 minutes, partly because I had not had any food in about five days. Then they gave me anti-diarrhea drugs (I think immodium or a variant) and this caused the opposite problem. They did not want to discharge me until I had a normal bowel movement and my white blood cell counts had started recovering. The way my doctors explained it, I probably would have had problems with gall stones 20-30 years from now, but the chemotherapy tends to cause all problems to happen all at once. While I was in the hospital I lost another 5 pounds, so the total weight loss is now 20 pounds. I am still neutropenic (reduced white blood cell counts), but there's no reason why I need to be hospitalized for this. While I was in the hospital they trained me to give myself my own Neupogen shots, so I will be taking care of this. Since I'm neutropenic, I need to avoid people (especially anybody who has been sick recently), flowers, fresh fruit and fresh vegetables and so on for a while. The only other major event is the wisdom tooth that needs to be extracted (and which we were hoping to avoid extracting) fractured Saturday morning and now definitely needs to be removed. This will happen sometime early this week. My platelet counts are still fine, so this shouldn't be a problem, but if it is a problem I will probably need to undergo a platelet transfusion before the procedure. My restrictions right now also include a prohibition on strenuous exercise, lifting anything more than 10 pounds, bathing until the incisions heal sufficiently (showers are ok), etc. My mother, who just retired, is flying in on Monday and will spend the next 4 weeks with us helping out. While I was in the hospital my hair started falling out faster because of the chemotherapy. If I grab a clump of hair with my fingers, it tends to come out very easily. Gray hairs and thinner hairs are falling out first. I'm also bruising very easily. The tinnitus also makes it difficult to sleep or concentrate enough to read. The hospital room was rather nice. I did not enjoy being on an IV all the time and the constant pokes and prods to draw blood. One time they drew blood three times in one hour because somebody didn't coordinate all the orders, and the first one had to poke me three times because he was having trouble hitting a good vein. The IVs were especially annoying. The machine that regulates the flow of IV fluid makes a clicking noise every second. Whenever the IV bag runs out of fluid or the IV line gets a crink in it, the machine starts sounding an alarm. There's a silence alarm button on the machine, but that works only for a minute. The only solution is to call the nurse to fix the machine, and it takes the nurse anywhere from 15 minutes to an hour to respond. Even when the machine is working, they are pumping so much fluid into you that you have to pee every 30 to 60 minutes. All this makes it very difficult to sleep for more than half an hour at a time. The bed, a Hill-Rom Advance Series Bed, is a very cool piece of technology. The firmness automatically adjusts according to pressure to minimize pressure, so it is a very comfortable bed. It also does all the usual contortions of a hospital bed (i.e., you can put it into a sitting position). The nurses can also use it to weigh you while you're in bed.
|
||||
| June 30, 2003 (Monday) |
The second pathological opinion from Indiana University Medical Center
came in today, and it confirms that there are no nonseminomatous
elements in the testicular cancer.
My hair loss is accelerating. A good deal of hair is now missing from the back of my head. Previously the back of my head was completely covered with hair, with only pattern baldness on top. The hair loss is more akin to severe thinning than complete baldness right now, since there is still some hair, just not all that much of it. Enough hair is missing that the back of my head now feels cooler, so I will definitely need to wear a hat. My wife says the hair loss looks like mange. I will probably shave my head later this week, since that will look better than the intermediate result.
The appointment with my oncologist brought some really good news. They measured my counts in the office, and my white blood cell counts are 4.8 (they ran the test twice), so I'm no longer neutropenic. (A WBC of 4.8 is within the normal range. Before chemotherapy my count was 8.4 to 9.3, so this is still below normal for me, but it is within the normal range. I will have one more shot of Neupogen tomorrow, and that's it unless my counts drop again.) My oncologist also said that my tumor markers have dropped to zero. This means that the cancer is responding to treatment. He is going to delay the start of the next cycle by a week, to give my body time to recover from the surgery. He wants me to have a hearing test before the start of the next cycle, because my tinnitus is so severe. If the ENT confirms hearing loss, he may want to substitute carboplatin for cisplatin. Although carboplatin isn't as effective as cisplatin for non-seminoma, it has been successfully used for seminoma patients and has significantly reduced ototoxicity. He is also talking about possibly reducing me to two cycles instead of three, depending on the results of the PET scan and other diagnostic tests. My broken wisdom tooth is scheduled to be extracted tomorrow. The PET scan and Bleomycin are scheduled for Wednesday.
|
||||
| July 1, 2003 (Tuesday) |
More hair fell out last night, and what was left wasn't worth
keeping. I woke up with a lot of hair on my pillow. So I decided to
shave off the rest. A picture of the result appears below.
I started experiencing some bone pain today, presumably from the Neupogen. Since my last Neupogen shot was today, hopefully the bone pain will go away in a few days. My wisdom tooth was extracted today. It took only 2-3 minutes after they numbed me up with novocaine. The novocaine numbed me all the way to my left eyeball, so I didn't feel a thing. I took a percoset when I got home during the first gauze change. The old wives tale about using a wet teabag to help with clotting does help. The oral surgeon had a neat piece of technology in his office. Instead of taking X-rays the old fashioned way, by forcing you to bite on a film positioner, he has a device that rotates about your head taking X-rays of your entire mouth all at once. You still have to bite onto a positioner to keep your head from moving, but it isn't as bad as having bulky film in your mouth. Since the machine is carefully calibrated, you don't need to wear a lead-lined shield to protect you from stray X-rays.
|
||||
| July 2, 2003 (Wednesday) |
The bone pain has gone away.
I had a negative reaction to the Bleomycin today. It gave me the shakes and chills. I didn't have a fever, however. The shakes and chills went away after about 4-5 hours. Since I didn't have this last time, I think the fact that I was fasting for the PET Scan may have had an impact. It certainly caused my fatigue to become more severe. Today I had the PET Scan. First the nurse installed an IV. Then she installed a urinary catheter. The latter is necessary because the radioactive sugar they use during a PET Scan collects in the bladder, so they need to flush the bladder while the PET Scan is proceeding (not because of a radiation risk, but to allow for the imaging of that part of the body). The last time I had a catheter installed, I was unconscious under general anesthesia. This time I was awake, and it hurt quite a bit. I was then wheel-chaired to the PET Scan facility. This consisted of the equipment mounted in a trailer. The equipment is fairly expensive, so several hospitals share the equipment. This is why West Penn Hospital only conducts PET Scans on Wednesdays, since the trailer is parked outside their nuclear imaging department only on Wednesdays. About 45 minutes before the PET Scan they injected a radioactive sugar through the IV. Since I was fasting that day, my blood sugar levels were lower, allowing the radioactive sugar to travel through the body. Parts of the body that are metabollically active then collect the sugar, causing them to show up on the PET Scan image. Cancer tumors are metabollically active, so this technique is useful for identifying active cancer sites. This can be helpful in staging the cancer (i.e., identifying whether suspected tumors found during a CAT Scan are actually cancer), detecting microscopic tumors below the resolution of a CAT Scan, and in determining whether tissue still contains cancer after treatment. The latter will be important later, since seminomas tend to become fibrotic tissue after treatment, meaning that they still show up on a CAT Scan after treatment is complete. Timing of the PET Scan is critical, since they must scan the body while the sugar is still radioactive (it has a very short half life). They divided the scans into six sections, taking about 5 minutes per section. When it was over, a nurse came in to remove the catheter. That hurt as much as the insertion, because they blow up a balloon in the catheter after it is inserted to prevent the catheter from slipping out and they didn't fully deflate it. I will probably not receive results of the PET Scan for several days, since it needs to be evaluated by a radiologist. I have no further diagnostic tests or treatments scheduled for the rest of the week.
|
||||
| July 5, 2003 (Saturday) |
The incision above my belly button opened up again on Friday and started
bleeding. It soaked through six changes of bandages over the past two days
before it started slowing
down enough to start clotting. I wasn't showing any signs of
infection, so the doctor didn't see any need for me to come in.
|
||||
| July 7, 2003 (Monday) |
My doctor examined the incision area and said that it was fine. There
was a little clear seepage while he was examining me, and he said that
that was normal. He
told me to change the bandages every four hours, to use clean gauze
to clean the area, and to use neosporin or bacitracin along the
incision line before putting on a fresh bandage. Some bleeding or
seepage is fine, so long as the seepage is clear and not discolored.
The PET scan showed no active disease in any of the sites from the CT scan. However, it showed significant bone marrow activity throughout the skeleton, presumably because of the Neupogen. It is possible that these findings represent a false negative because of the extensive bone marrow activity. As such, they are inconclusive. The radiologist is recommending a repeat PET study six weeks following the completion of chemotherapy. My doctor said that it is normal to feel fatigue at this point, and that I should take a nap in the afternoon if I feel tired. I've lost 2 more pounds in the past week, so my weight loss is slowing. He would have expected greater weight loss following the gall bladder surgery, so only 2 pounds is good. Must be my mother's good cooking.
|
||||
| July 8, 2003 (Tuesday) |
The hearing test was rescheduled for today since Dr. Barsouk wanted to
be sure to get the results before my next cycle. We had to drive all
the way to UPMC McKeesport Hospital for the test, and ended up
arriving late because the directions were bad and we had to take a 20
mile detour because of construction at the exit we were supposed to
take.
The audiogram did show some additional hearing loss. The right and left S.R.T. were 20 db and 22 db, compared with 5 and 10 db on an audiogram from 19 years ago. Discriminability is 100% at 60 db, compared with 100% at 40 db 19 years ago. So basically I have trouble hearing soft voices. The high pitch hearing loss has also become worse by about 10 db. The workaround is for me to tell people to speak louder when I have trouble hearing them. The tinnitus was much better today, not much worse than it was before the chemotherapy. So perhaps the tinnitus is temporary. The otolaryngologist recommended staying away from caffeine, alcohol, chocolate, and steroid medications (e.g., the decadron) to help minimize the tinnitus.
|
||||
| July 9, 2003 (Wednesday) |
The tinnitus was fairly strong when I first woke up, but then dropped
back to just above pre-chemo "normal" levels an hour or so later.
I also didn't have as much fatigue today. So hopefully the
chemotherapy side effects will all be temporary and will go away a few
months after I'm done.
Today is the last day for the horrible tasting antibiotics (Metronidazole). The pills are so huge (500 mg) that it's hard to avoid having them touch your tongue even when swallowing them with copious amounts of water. The bad taste then lasts for hours. I've lost a total of four inches of wasteline so far. If I lose much more weight, I'll have to buy all new clothes. I haven't needed to shave for the past few days. One of the few benefits of chemotherapy. One of our vacuum cleaners would constantly lose suction after the filters got clogged with cat hair. Rather than buy a run-of-the-mill vacuum, we bought a Dyson Animal (Purple). It finally arrived today. It's an expensive vacuum cleaner, but it works so much better than any other vacuum cleaner we've tried. The suction is much stronger, and it doesn't lose suction as it cleans. It took two extra weeks to arrive, because Amazon.com sent it by UPS to my billing address, a PO Box. (In a classic "blame the customer" move, Amazon said that it was my fault because I wrote "PO Box" instead of "P.O. Box" in my billing address, so their software couldn't tell that it was a PO Box. Maybe they need to hire better programmers, or at least address correct all their customer addresses. They still didn't answer why it was sent to my billing address, when I specified my street address as the shipping address. Amazon's customer service operation has gone downhill recently.)
|
||||
| July 10, 2003 (Thursday) |
Today I heard from a friend that the information I posted on a mailing
list about my cancer caused him to check out a testicular mass. It
turned out to be stage I non-seminoma. I'm glad that my email helped
him catch his cancer early.
The follow-up appointment with my oral surgeon was very quick and went very well. He said that I was healing fine from the wisdom tooth extraction. My tinnitus today was back to pre-chemotherapy levels. Also, I didn't have any peripheral neuropathy today. I also did not have much fatigue. All of these are good signs that the chemotherapy side effects will be temporary and not permanent. Today was the first insurance company glitch I've had to deal with. They classified the pulmonary function test as "HDO OUTPT HOSP OTHER", and deducted a $50 copay. They should have classified it as "HDM OUTPT HOSP DIAGNOSTIC". Diagnostic tests do not require a copay. I called them and asked them to correct the error. I noticed that I get the "Explanation of Benefits" statements about a month after the actual procedures.
|
||||
| July 11, 2003 (Friday) |
Today was the two-week follow-up appointment for the gall bladder
surgery. The doctor said that draining in the incision area is normal,
and that I should expect it to continue to drain for another three
weeks. He said that instead of using large gauze bandaids, I should
use absorbent gauze folded over and taped. This would absorb the
draining fluid better. (The large bandaids I was using had a tendency
to leak, especially when I sleep on my side.) He also told me to "milk"
the incision every time I changed the gauze to get the built-up fluid
out. He replaced the upper two bandaids with fresh steri-strips (these
were healing well), saying that I would not need to change them. He
also replaced the lower right large bandaid with a smaller bandaid,
saying I should change it as needed. He scheduled a follow-up
appointment for three weeks from now.
There was no co-pay for this visit because my insurance apparently doesn't require a co-pay for follow-up appointments within 90 days of surgery. Dr. Semins said that it is ok for me to drive again, although I should continue to refrain from picking up anything that weighs more than 5-10 pounds.
|
||||
| July 14, 2003 (Monday) |
Today was the start of my second three-week cycle of chemotherapy.
The antinausea medication they gave me (Zofran) caused a burning
sensation along my vein. Since this was the second time this happened,
they switched me to Kytril, a different antinausea medication. That
stopped the burning. They told me I could continue taking the Zofran
pills that evening, but I should try it without the Decadron (a
steroid) to see if it was enough. The purpose of the Decadron is to
enhance the antinausea capabilities of Zofran. But since I had a
negative reaction to the Decadron on day 5 of the first cycle, it
would be helpful to see if I can get away without the Decadron.
They had cable TV installed in the treatment room today, so the TV is no longer limited to the on-air network TV channels. I was able to have CNN on in background while I worked offline on my laptop. I also spent some time reading a science fiction book by Brin (Kiln People). My counts were all fine. In fact, my white blood cell count was 8.3 mIu/ML, which is solidly normal. My insurance company called today to let me know that the $50 copay on my pulmonary function test has been "waived", their way of saying that I was right that it should have been classified as a diagnostic test and so not subject to a co-pay. In the meantime, I got the explanation of benefits from the first meeting I had with my oncologist, and it showed him as being out-of-network. Since I called the number on the back of my card that day to verify him as in-network, and also have printouts from the insurance company's web site showing him as in-network, I called to file an appeal. I've even got witnesses, since I called the insurance company from my urologist's office while my urologist called the oncologist to also verify that he was in-network for my insurance. Since this means a difference of $3,900 in my out-of-pocket expenses, I'm definitely appealing. I wonder whether the insurance company is deliberately incompetent or whether they just hire morons. Incidentally, the insurance company also made an error on a urinalysis, coding it as "pay to patient" instead of "pay to doctor". Since it was only $6, I deposited the check and paid the corresponding urologist bill for $6. That was simpler than waiting on hold for half an hour for the insurance company.
|
||||
| July 15, 2003 (Tuesday) |
The Kytril was much more effective at stopping nausea. Not only didn't
I have any nausea, but I also had an appetite. Of course, it could be
that this was not due to the Kytril alone, but because I also had a
little bit of Zofran before the nurse stopped the IV because of the
burning sensation. So I'll see today whether it continues to be as effective.
I still took a Zofran tablet in the evening. Last night I skipped the Decadron tablet (with doctor's approval) and was fine. Decadron is supposed to enhance the antinausea effect of Zofran. But since a Decadron shot caused me to vomit on day 5 of the first cycle, and because my doctors thought that the Decadron may have contributed to my pancreatitis and abdominal pain, it was decided to see how I react to skipping the Decadron in the evenings. My nurse pointed out that nausea tends to increase as the week progresses. I did have some nausea this evening. Today I got poked three times. The first time missed the vein. The second time hit the vein, but the vein did not have good blood return. Third time worked. An interesting hair loss observation. You don't lose hair from every region of your body to the same degree. In some areas the hair is just more sparse (e.g., eyebrows, upper chest and belly) and in some areas it is completely gone (e.g., head, pubic region) and in some areas there is no change (e.g., legs and arms). Even in those areas the hairs are a little thinner, and some of the hairs will come out easily. Also, even in the areas with hair loss, the hair is still growing back in, but the new hairs shed a lot. Looking at the hairs that didn't fall out, I can see that they start out thick, and then suddenly become thinner. I haven't needed to do anything to the hair on my head since I shaved it off two weeks ago. I also haven't had to shave my face since then; the five-o'clock shadow comes off when I shower. Eyebrows are still there, but they've thinned a little. Apparently they sell specialty wigs called "merkins" for folks who lose their pubic hair. This is incredibly humorous. Is there really a market for such things? I can understand wearing a wig or a hat to insulate the head from cold air in wintertime. But a wig for one's nether regions?
|
||||
| July 16, 2003 (Wednesday) |
The nurse was right. Last night I had some nausea, but the Zofran
tablet seemed to help a bit. But then I woke up this morning at 5 am
with nausea. I didn't vomit, but it is about as strong as it was on
day 4 or day 5 of the previous cycle of chemotherapy. My blood
pressure is also up a bit.
At the hospital they gave me Kytril and Decadron right away. It took the edge off the nausea, but there was still an undercurrent of nausea throughout the day. As soon as I got home I took a Zofran and Decadron. I'm also going to switch to the BRAT diet (Bananas, Rice, Applesauce, Toast), which is supposed to help with nausea. I was so nauseous that I was unable to get any work done while at the hospital. I read the newspaper, but was unable to start a science fiction book, and the TV was too boring. I tried sleeping a bit, unsuccessfully. Today was a four-poke day. The first needle couldn't find the vein. The second needle worked, but then the vein dried up about an hour before I was done with chemotherapy. So the nurse tried the other arm. The third needle missed the vein. So then she tried the veins on the back of my left hand. That one worked. Since I still have hair on the back of my arms, she used a clingy bandage that sticks to itself instead of tape to cover the needle hole with gauze.
|
||||
| July 17, 2003 (Thursday) |
I almost vomited last night, twice, and almost once this morning. The
nausea is getting pretty bad. So far I've been able to avoid vomitting
through will power, but that won't work much longer.
The peripheral neuropathy and tinnitus are back. I've also lost all the weight I gained last week, so I'm back to having lost 23 pounds since the orchiectomy. Today was a one-poke day. My oncology nurse switched off with a different oncology nurse since sometimes different nurses are better at finding different veins. This time it worked. (I've been holding the veins on the back of my hands, which do pop out well, in reserve for the third cycle, to ensure that I avoid the need for a port-a-cath or picc line.) They prescribed Ativan (Lorazepam) for me to take for the nausea in the evening. It helped a lot, but it also knocked me out. I took one around 6 pm and one around midnight. I missed dinner as a result. (Not that I would have been able to eat anything anyway.) So as of Friday morning, I've lost another 2 pounds, bringing the total to 25 pounds. I'm going to stick with the BRAT diet, plus some liquid diet (soup broth, jello, etc.).
|
||||
| July 18, 2003 (Friday) |
Upon arriving at the hospital this morning, I promptly vomited. It was
mostly the vegetable broth soup I had had for breakfast. The nurse
told me to take plenty of Ativan this weekend to try to sleep through
the worst of the nausea. I have no appetite.
Other than that, today was a one-poke day.
|
||||
| July 19-20, 2003 (Saturday-Sunday) |
Despite taking Zofran, Decadron and Ativan continuously, I had nausea
all the time this entire weekend. There was also a taste change in the
back of my throat that made lemon candy intolerable. The Ativan made
me sleep through a lot of it, but one can only sleep for so long. This
is pure torture. I constantly feel like I need to vomit.
I ultimately did vomit at 8:30 pm on Sunday, in the bathroom sink. Vomitting never makes you feel better.
|
||||
| July 21, 2003 (Monday) |
My follow-up audiogram went well, showing only mild deterioration in
hearing loss, well within the variation from test to test. My
otolaryngologist does not recommend changing the chemotherapy protocol
as a result, but does recommend having a follow-up audiogram about a
month after chemotherapy is over.
My follow-up appointment with the urologist also went well. He said that my incision area has healed well (the healing ridge is gone), and that unless any of the followup CT scans or X-rays shows a problem, he won't need to see me again. At the oncologist they gave me Neulasta, a variant on Neupogen. This caused me severe bone pain. I tried napping through it and the nausea, without success. I vomitted twice Monday evening, once at 10 pm and once at 11:30 pm, and was not able to sleep all night.
|
||||
| July 22-24, 2003 (Tuesday-Thursday) |
I was hospitalized on Tuesday (discharged Thursday) because of severe
bone pain, severe abdominal pain and severe nausea. I vomited several
more times while at my oncologist's office.
The severe bone pain was caused by the Neulasta working too well. It caused the bone marrow in my back and sternum to overproduce white blood cells, causing the white blood cell count to far overshoot normal levels. It took until Wednesday for the white blood cell counts to drop to 12.3, which is about 30% above normal. The abdominal pain was assumed to be related to the nausea, which itself was delayed nausea from the chemotherapy. X-rays showed no problems in the abdominal area. So the doctors kept me in the hospital on IV fluids, liquid-only diet and anti-nausea medication until I recovered. They started me back on semi-solid food on Wednesday, and decided to keep me overnight to make sure I was back to "normal". (Unfortunately, the hospital kitchen staff apparently had only one kosher meal available -- lasagna -- so I had the same thing for lunch and dinner Wednesday and lunch on Thursday.) While I was in the hospital the first IV backed up, causing a lot of swelling in the right arm. This also caused a lot of bruising on my right arm. The nurse put a hot compress on it and the swelling went down after about a day. They switched me to an IV in the left arm, using a vein in the muscle. I hate IV fluids, because they pump so much fluid in you that you have to pee every half hour. But they doctors say that it is important to pump a lot of fluid through you after chemotherapy so that you don't suffer from kidney failure. My tinnitus is back, much more severe than before. I talked with one of the oncologists about how to avoid this happening again next cycle. He said there's a new anti-nausea medication they can try. He said he'll also discuss with my oncologist about admitting me to the oncology ward for the last day of chemotherapy plus a few days, so that I'm not in severe nausea over the weekend. (Also, when they admit me to the hospital in a hurry, they can never get me a bed in the oncology ward. This means that the nurses have less experience with anti-nausea medication, and have to go get it instead of having it readily available on the floor. This causes delays in getting me the anti-nausea medication.)
|
||||
| July 25, 2003 (Friday) |
I started having nonstop diarrhea at 4 am. If I drank some water, it
came out the tush a few minutes later. Other than that, my vitals are
fine and I'm feeling good. I called the oncology nurse when she
arrived in the office in the morning, and she said I could take
immodium. That seems to have worked. I'm drinking pedialyte to replace
the lost electrolytes (I hate Gatorade, so pedialyte is a tolerable
substitute).
The oncology nurse called back an hour later, saying that my oncologist would like me to come in to give a stool sample, since he's concerned that my diarrhea might be due to an infection. But when I said that it was just like the last time I was hospitalized, and that the immodium seems to have worked (so I have no sample to give), and that my diarrhea smelled normal (i.e., not foul), she agreed to let me skip giving the sample, so long as I continued to be ok. She said that if anything changed, I should come in immediately. I really don't want to spend the weekend in the hospital, and I'm convinced that this is just like the last time, when my digestive system took a while to reset after not having any solid food for a while. I have a few interesting observations about hair loss. I haven't had to shave my face or head since the beginning of July. This isn't really because my hair has stopped growing, although it is growing more slowly. But it seems that whenever I shower, the stubble on my face comes off with the dirt. Today I noticed that there is some hair growing on my upper lip, but it is much finer than previously and the hair is almost completely transparent. While I was in the hospital my son started 'talking'. If you talk to him, he'll gurgle back and try to hold a 'conversation'. He has also started sucking on his fists, although he hasn't yet opened his hands while sucking on them. It will be interesting to see whether he becomes a thumb sucker or a finger sucker.
|
||||
| July 26-27, 2003 (Saturday-Sunday) |
Friday night I started having bone pain again. It occured in three
places: the base of my back, the sternum, and in my right leg. I'm not
sure the latter is related, as it wasn't in the thigh but in a diffuse
region on the right side of the knee. I called the oncologist on call
and he said I should take two oxycodone (I had some left over from
after the gall bladder surgery) and to call again in the morning if
the pain didn't improve. I still had bone pain in the morning, but it
wasn't as bad. My wife gave me a back massage, but said that the
chemotherapy drugs in my sweat caused her hands to tingle. So next
time she's using disposable gloves.
I'm experiencing taste changes for the first time. My saliva has a chemical taste. Also, I made some tuna fish with mayo and thousand island dressing (one of my favorite concoctions) and couldn't stand the taste. It tasted salty. I also can't stand lemon juice any more. Caffeine free Dr. Pepper still tastes great, even without the fizz. I had some falafel and pizza for brunch. I still have bone pain Sunday evening, but just in my back. My legs (calves) feel a bit weak when I stand or walk. I think this is related to the bone pain I had in my legs earlier. I'm drinking a lot of water in order to flush the chemotherapy drugs from my system. I don't want it to build up in my kidneys. So it's a constant drink-pee-drink-pee cycle. My pee no longer smells like battery acid, the bruises I got in the hospital are almost gone, and the peripheral neuropathy is almost gone, so this idea seems to be working. But I still have the tinnitus and hearing loss. The hearing loss is the equivalent of 20-30 db, according to a sound meter I used to measure the TV volume setting.
|
||||
| July 28-29, 2003 (Monday-Tuesday) |
The pain in my calves (more of an ache or soreness than pain) is not
bone pain, but muscle pain. My oncologist
says that this is a common side effect of chemotherapy, and it should
go away when I'm done with chemotherapy. I will just have to walk
through it.
My oncologist thinks that my delayed nausea after each 5-day course of etoposide and cisplatin may be due to underdosing of my Zofran. He wants me to take one 8mg pill three times a day instead of two times a day. The CVS pharmacy did not have enough Zofran on hand to fill the prescription, so they're going to have to order it. It should be in by tomorrow afternoon. My oncologist continues to believe that three cycles of BEP is overkill in my case, but he acknowledges that there is a statistical benefit to three cycles. So we are going to do the third cycle. He is warning me, however, that the third cycle will be by far the worst as far as side effects are concerned. We discussed the bone pain from the Neulasta. He says it is very unusual for someone to have more side effects with Neulasta than with Neupogen. He wants to keep me on Neulasta, however, because the drug is self-regulating to some extent. In other words, when it produces too many white blood cells, those cells help excrete the drug, bringing down the white blood cell count to normal levels. He prefers this to the hit or miss approach with Neupogen. To deal with the pain, he says they'll put me on a morphine drip in the hospital or give me oxycontin. My oncologist wants me to consider delaying the third cycle by a week. The way he described it was "I don't want you to come out of this a criple; don't try to be a superman." We agreed to meet on Monday, August 4, to discuss it further. If I'm back to "normal" (where normal has a surreal definition for cancer patients), he'll let me start the third cycle on Tuesday, August 5, otherwise he'll want me to wait a week to start on August 11. The other issue we discussed was admitting me to the hospital for part of the third cycle. He said he wants to admit me on day 3 of the third cycle, give me day 4 and day 5 of chemotherapy in the hospital, and then keep me in the hospital for 2-3 days after that. That way they can monitor my nausea more closely, ensure that I get anti-nausea drugs round the clock, and give me the new anti-nausea medication if necessary. This will also allow them to give me pain medication for the bone pain. The goal is to avoid having my digestive system shut down because of chemotherapy, nausea and vomiting. In other words, better to admit me to the hospital in advance than to have to admit me as an emergent case. This way they'll be able to reserve a bed in the oncology ward, so I'll get better care.
|
||||
| July 30, 2003 (Wednesday) |
At my oncologist's recommendation, I started taking the 8mg Zofran
pills once every 8 hours instead of once every 12 hours. Not only
doesn't this seem to be working, but it gave me a very painful headache.
On a scale from 1 to 10, where 10 is the most painful headache I have
ever had, it was a 45. It was far worse than any migraine I have ever
had. I called my doctor who told me to stop taking the Zofran. He said
that there is nothing I can take for the headache, and that I would
just have to wait until the drug had flushed from my system. So I
spent the afternoon in bed. The headache started dissipating at 8
pm, around the time I would have taken the next Zofran.
Also, probably unrelated, some of my joints have started occasionally 'popping' (akin to when you crack your knuckles). It isn't painful, just something new and different.
|
||||
| August 1, 2003 (Friday) |
The surgeon who diagnosed and treated my pancreatitis (and also
performed the gall bladder removal) says that I now have diabetes
caused by the pancreatitis. A urinalysis showed a 4+ glucosuria
reading. He said that the diabetes is probably permanent. I have to
have a bunch of blood tests, including a fasting blood sugar test (so
I can't do it today). I've scheduled an appointment with my PCP to
review the test results and learn about diabetes management.
Until I've met with my PCP, the doctor says that I should keep the carbohydrates to a minimum. So instead of the BRAT diet, which is high in starches (bread, spaghetti, etc.) I should eat a high protein diet, such as scrambled eggs, hot dogs, hamburgers, chicken, and turkey. Of course, such a diet doesn't help the nausea. The good news is I'm actually feeling pretty good today. No real nausea, although I have a loss of appetite and a bad taste in my saliva. The tinnitus is also only moderately severe today.
|
||||
| August 4, 2003 (Monday) |
I met with my oncologist today. We decided that I would start my third
cycle of BEP tomorrow. He had been leaning toward delaying it by a
week, but decided that I was well enough that a week's delay was not
necessary. He did, however, have the oncology nurse give me two bags
of saline through the IV today, since he thought I was a little
dehydrated.
The results of my blood tests came back, and weren't good. My blood glucose and cholesterol levels have gone haywire. (There is some evidence in the literature that cisplatin-based chemotherapy can cause hyperlipidemia.) My blood glucose levels are 184 (normal is 70-109), my 2-hour post-prandial glucose levels are 358 (normal is < 200), and my hemoglobin A1C is 8.1 (normal is 4.4 - 6.1). My cholestoral levels are 238 (normal is 120-199, two months ago I was 206), triglycerides are 248 (normal is < 150, two months ago I was 142), HDL cholesterol is 43 (normal is 40-59, two months ago I was 47), LDL cholesterol is 149 (normal is 60-129, two months ago I was 131), and my LDL/HDL ratio is 3.47 (two months ago I was 2.79). Tuesday and Wednesday I will receive my chemotherapy on an outpatient basis. I will be admitted to the oncology ward on Thursday and receive my chemotherapy on Thursday, Friday and Saturday in the hospital. They will keep me in the hospital through Monday or Tuesday. This will allow them to monitor and treat my nausea, try a new anti-nausea drug on me if necessary, give me insulin for the diabetes, and give me pain killers for the bone pain. They also want to keep my hydrated to prevent kidney failure. While I'm in the hospital they will bring in an endochrinologist to consult on the diabetes. There seems to be some disagreement about the cause of the diabetes. The surgeon who diagnosed the pancreatitis and performed the gall bladder surgery thinks that it was caused by the pancreatitis and is therefore permanent. My oncologist thinks that it was induced by the Decadron (a steroid) they've been giving me for nausea, and therefore temporary. My PCP says that my hemoglobin A1C levels indicate to him that it is permanent. Hopefully the endochrinologist will be able to shed some light on the matter. In any event, the management of the diabetes is the same, so today I have to go buy a blood glucose meter (my PCP is recommending the One Touch UltraSmart Meter Kit with built-in log book).
|
||||
| August 5, 2003 (Tuesday) |
The first day of chemo in the third cycle went well. The oncology had
a little trouble putting in the IV, but fished around a bit with the
needle until she found the vein. So today was a single poke day.
They are having me take Compazine in addition to Zofran and it seems to be working well. I have minimal nausea and no side effects from the Compazine. On the other hand, this is the first day, and cisPlatin tends to result in delayed nausea. My PCP explained that the high Hemoglobin A1C tends to be a long-term measure, and so elevated levels are an indication that the diabetes was on its way before I started chemotherapy. He did acknowledge that some folks believe it represents blood sugar levels over 6 weeks instead of 6 months. He also said that the pancreatitis and decadron could have accelerated matters. So now I have three different doctors telling me three different things:
From my understanding of Hemoglobin A1C, it measures the amount of glucose that has bonded with red blood cells. This reflects the blood sugar levels over the lifetime of the red blood cells, which is 2-3 months. That is more in keeping with the timeframe of my chemotherapy, which started almost 2 months ago. Also, my urologist did the same urinalysis tests multiple times (all before the pancreatitis), and none of them showed glucosuria. So I'm more inclined to believe my oncologist (who also specializes in hematology) and the surgeon more than my PCP. But we'll see what the endochrinologist says. The cause of the diabetes can have implications for treatment. For example, if it was caused by the pancreatitis, then insulin shots might be warranted. If it was caused by long-term development of insulin resistance, insulin shots wouldn't necessarily help. Managing my diet and spreading out carbohydrate intake more evenly throughout the day will probably help for all diagnoses, as will exercise and weight loss. My PCP gave me a basic education about managing diabetes. I'll need to get more information. For example, I'd like to find a web site that lets you specify your favorite meals, and then assembles them into a set of daily/weekly menus that help manage your blood sugar levels. If I can't find such a web site, I'll have to implement my own. It would actually be kind of fund to implement, since I could try multiple optimization methods (e.g., hill climbing, simulated annealing, simplex method, depth-first search, and genetic algorithms). I also need to find a few good diabetic cookbooks. My PCP is also recommending that I increase my exercise regime and lose an additional 30 pounds. The One Touch UltraSmart glucometer is an interesting gadget. It's like a fancy PDA in many ways. In addition to testing blood glucose levels and storing the results in a built-in logbook, it lets you record blood pressure, height, weight, hemoglobin A1C, doctor visits, exercise, meals, and so on. You can also upload the data to a computer for printing graphs and charts.
|
||||
| August 6, 2003 (Wednesday) |
Today I measured my glucose levels for the first time. They were 204
before breakfast, 337 before dinner. I also asked my oncology nurse if any
of my previous blood tests included glucose levels (obviously
non-fasting), and she said that on June 2 I was 154 and on June 23
183. The finger pricks weren't bad, but I suppose that they will
quickly become annoying after the novelty wears off and my fingers
build up calluses.
I haven't yet figured out where I'm going to carry the glucometer. Right now I carry too many gadgets and things with me. I've got a Palm Pilot, cell phone, business card case and digital camera in one pocket, and a wallet, money click, and pen in the other. Keys are in a third pocket. I may need to replace the Palm Pilot and cell phone with a Handspring Treo 600 to make room. But I was holding off on getting a Treo until they improved the battery life, since I don't like having to recharge the unit every day. (My current cell phone and Palm Pilot can go a week before needing to be recharged.) Today was a two-poke day. The first attempt to start an IV was in the most popular spot on my right arm. Although it initially worked, the flow stopped a few seconds later. She wrapped a warm towel around my forearm, and that caused another vein to pop to the surface. It is encouraging that so far they haven't needed to resort to IVs on the back of my hand. I had a little more nausea today. This was probably partly due to my last Compazine pill being taken at midnight, partly due to the Kytril not being as effective, and partly due to it being day 2. The nurse also told me that they may not be able to get the Emend (the anti-nausea medication for break-through nausea) from the hospital formulary tomorrow, but they've got other tricks up their sleeves. I'm quite certain that I'm going to have break-through nausea again this cycle. I will be in the hospital starting tomorrow and running through Tuesday, so there will be no entries in the chronology until I am discharged.
|
||||
| August 7-12, 2003 (Thursday-Tuesday) |
For whatever reason they weren't able to get the Emend from the
hospital, but the local CVS had it in stock so they called in a
prescription and my wife picked it up. The Emend works very well, and
was able to control my nausea. Between the Emend, the Compazine, and the
Kytril, I had less nausea this cycle than the last. My fatigue is much
more severe, however. I am totally lacking in energy. I also have
absolutely no appetite.
While I was in the hospital the Joslin Diabetes Center nurse came by to provide diabetes education. That was quite helpful. The Decadron definitely has an effect on my glucose readings. My glucose readings are 100 to 150 points lower without the Decadron. I feel really horrible. My doctor says that the next few days will be the worst. I asked about going back to the hospital, but he said there isn't anything they can do to make it more tolerable. I have an appointment to see him Thursday, and to get the Bleomycin.
|
||||
| August 13, 2003 (Wednesday) |
The tinnitus and peripheral neuropathy are back full throttle, worse
than before. I tried eating some scrambled eggs for breakfast, and it
tasted like I was eating foam rubber. But at least I was able to keep
it down. I've lost a total of 38 pounds to date.
I'm still physically weak and without any energy, but things seem a little better this morning than they were yesterday. But not much better. I can't do anything -- I have a 60-second attention span. The various anti-nausea medications only take the edge off. Between that and the diarrhea, I'm constantly visiting the bathroom or drinking pedialyte.
|
||||
| August 14, 2003 (Thursday) |
My oncologist had me provide a stool sample to make sure I hadn't
picked up an infection that was causing the diarrhea. They won't know
the results for a few days. In the mean time he prescribed
flagyl. They'll call me with the results, which will entail either
increasing the dosage or stopping it. He also prescribed immodium.
They gave me kytril for the nausea and hydrated me for several hours before giving me the Bleomycin. Between the nausea and diarrhea, I couldn't sleep. I also had a pretty severe case of acid reflux, but Tums handled that. The nausea seems to have abated somewhat by 2:30 am Friday. I still have it, but it isn't as bad. Well, my saliva tastes bad, and makes me want to vomit every time I swallow. We talked about my undergoing physical therapy and joining a gym. He wants me to do this, but not until he gives his ok.
|
||||
| August 15, 2003 (Friday) |
I discovered a drawback to weight loss today. I've lost enough weight
that there isn't much fat around my hips. This makes lying on the floor
painful on the hips. I still have enough fat on the tush that sitting
isn't a problem, although it is less comfortable.
I've decided that instead of getting a Segway, I'm going to get a lot of little gadgets. For example, I bought an Epson TM-U300PD receipt printer and an AirClic barcode scanner, and will create a shopping list printer for the kitchen computer. I'd love to have a Segway, but the shopping list printer and similar ideas are much more practical and less expensive.
|
||||
| August 17, 2003 (Sunday) |
The weight loss is causing problems in other areas. I no longer have
any cushioning around my knees. Previously, I would sleep on my side
with my legs together. Now, my knees bump against each other somewhat
painfully. So I have to sleep with a blanket between my legs.
The nausea seems to be gone, except when I get the bad taste in my mouth. The bad taste comes and goes. It is especially bad in the morning or when I lie down. The taste is in my saliva. When I swallow the saliva sometimes it makes me nauseous. Brushing my teeth or eating a breath mint seems to help reduce the taste for an hour or so. Drinking a lot of water also seems to help. The tip of my tongue tingles or is numb. This is probably related to the taste changes. I still have peripheral neuropathy and tinnitus. My arms also hurt a bit, especially where all the IVs have gone in. I feel like I have passed through purgatory and barely survived to return to the land of the living. The chemotherapy for testicular cancer is one of the most effective forms of torture ever devised by mankind.
|
||||
| August 18, 2003 (Monday) |
The oncologist's office called to say that the stool sample culture
came back negative, so I didn't pick up an infection in the
hospital. They told me to stop taking the Flagyl.
|
||||
| August 19, 2003 (Tuesday) |
I woke up this morning with really bad peripheral neuropathy. I still can't
feel my fingers, but at least I can type again. I also had some really
deep bags under my eyes, severe fatigue, and a bad taste in my mouth.
Later in the day I got a very severe migraine. It was unlike my normal migraines, in that it was on the right side (normally mine are on the left) and had severe nausea associated with it (normally the nausea, if any, is very mild). I also had minor nosebleeds in both nostrils. I'm pretty certain it was a migraine because I had a heightened sense of smell, which always happens with my migraines, and it responded to Amerge. It was similar in some ways to the Zofran migraine I had previously. I gained 10 pounds in the last two days. Some of this is rebound from the diarrhea (i.e., water weight gain). The rest is not watching how much I ate while recovering from diarrhea.
|
||||
| August 20, 2003 (Wednesday) |
I woke up at 3 am for an unknown reason and couldn't get back to sleep
until 5 am. I woke up again at 9 am with a residual migraine. I wonder
if I'm suffering from some kind of Zofran withdrawal.
I still have severe peripheral neuropathy. Taking a very hot bath helps. The vein pain in both arms seems to have gone away. I can't say the same for the bad taste in the mouth nor the tinnitus. My weight has stabilized, losing a pound from yesterday. At this point I've lost a total of 26 pounds since the day after the orchiectomy. My blood glucose levels this morning were 135 (top of the normal range). I guess having spanish rice for dinner helped. I had skipped measuring glucose levels while I was recovering from the diarrhea.
|
||||
| August 21, 2003 (Thursday) |
I had another migraine starting last night around midnight. This one
was a more normal left side migraine, but more intense than my usual
migraines. The Amerge also only took the edge off the migraine,
leaving behind a still nasty headache with nausea. I was only able to
sleep for 3-4 hours, and when I woke the migraine was still present.
Today was my last day of Bleomycin. It took three pokes to find a vein that wouldn't dry up. My white blood cell counts were low (1.1), so I'm neutropenic and will be taking Neupogen for the next few days. I'm also somewhat anemic, but not enough to warrant taking Procrit. I pointed out to the nurse that I had developed freckles at each of the IV sites, and she said that it is common for patients receiving Bleomycin. It is called "chemo burn" and may fade a little with time. That probably explains why all the scars from my surgeries are dark. I noticed today that my eyebrows have thinned out considerably. They're still there, just not as bushy or prominent as before.
|
||||
| August 22, 2003 (Friday) |
Today was my second day of Neupogen, and the bone pain is back.
It is just in my back, but it is pretty severe.
|
||||
| August 23, 2003 (Saturday) |
I had to take two oxycodone pills last night because of the bone pain,
which is now in both my back and sternum. The pills dulled
the pain enough so I could get some sleep.
The doctor said that the pain is an indication that it is probably safe to skip the last Neupogen shot. He said that if I wanted, I could take some additional pain medication along with the last Neupogen shot. But I'm all out of oxycodone, and one can't call in a prescription for that type of medication. So he said I should monitor my temperature and watch out for signs of infection, and call him again if my temperature goes above 100.5 (it's 98.1 right now).
|
||||
| August 24, 2003 (Sunday) |
I'm still feeling slightly nauseous, but there's no migraine. If the
nausea is coming from the Bleomycin (a first for me) hopefully it will
go away in a few days.
The bone pain is starting to go away. I tripped on the sidewalk near my house (there's a two-inch drop at the edge of the sidewalk), scraping my knee pretty badly. It seems to have clotted ok, but is still red and painful. I'll show it to my oncologist at my appointment on Monday.
|
||||
| August 25, 2003 (Monday) |
My white blood cell counts were 8.6, so I'm no longer neutropenic. I
am, however, still anemic, and my red blood cell counts were low
enough that they decided to give me Aranesp. (Aranesp is like Procrit,
but lasts three times longer, so only one shot is usually required.) That stuff really stung
badly going in. Hopefully my red blood cell counts will go up by the
time they need to give me the second shot, so I can avoid the sting.
They also drew blood for checking my tumor markers (beta HCG). They'll call me with the results a few days from now. It took them four pokes to find a vein they could use to draw the blood. The hospital will call me to schedule the follow-up CT scan (about two weeks from now) and PET scan (about six weeks from now). The PET scan is delayed to allow time for the Neupogen to get out of my system. My oncologist said I can travel again, so long as I schedule any travel around my appointments. I've officially lost a total of 30 pounds from start to finish.
|
||||
| August 26, 2003 (Tuesday) |
My CT scan has been scheduled for September 9, in the morning.
Today my primary complaints are: peripheral neuropathy (especially in my fingertips), bad taste in my mouth, tinnitus, and slight nausea.
|
||||
| August 27, 2003 (Wednesday) |
The incision above my belly button started oozing again, but quickly
scabbed over. Otherwise nothing much happened today. I still have
peripheral neuropathy, tinnitus and light nausea.
|
||||
| August 28, 2003 (Thursday) |
Good news. I got a copy of the lab results for beta HCG (my tumor
marker) and it shows a normal level of <5 mIU/mL. This is an
indication that the chemotherapy was effective against the cancer. We
won't know for certain that the cancer is gone until the CT and PET
scans.
|
||||
| August 31, 2003 (Sunday) |
While grocery shopping, the incision above my belly button started
oozing again. I wasn't doing anything strenuous -- no heavy lifting,
no bending at the waist -- so I have no idea what could have caused it
to start oozing. There was a fair amount of pus, so maybe the pus had
been building up pressure until it popped. When I got home I 'milked'
it to get the rest of the pus out, then put on a fresh nonstick
bandage.
|
||||
| September 3, 2003 (Wednesday) |
The incision is still seeping, but it doesn't seem infected.
The scab on my knee is starting to come off, with new skin underneath, so my platelet count must be ok. My eyelashes are falling off, so I'm still losing hair. My eyebrows have also thinned out to a faint shadow. I have a greater tendency to sunburn. It isn't painful (no itching), but I've been peeling even after a slight exposure. I've also gotten a few new freckles, especially where they poked me with an IV. (My orchiectomy scar is also dark brown.) So far I've been told that I look like each of the following celebrities: Paul Shaffer, the three curious characters from Blue Man Group, and Lex Luthor (Michael Rosenbaum). Decide for yourself.
|
||||
| September 5, 2003 (Friday) |
A limited amount of facial hair has started growing again, mostly on
my upper lip. The mustache hairs are coming in transparent instead of
dark brown.
The incision over my belly button is still not healing completely, I still have tinnitus and peripheral neuropathy, and I still have occasional mild nausea.
|
||||
| September 8, 2003 (Monday) |
I figured out that the belly button incision was continuing to seep
because the bandage was preventing it from forming a scab. More
accurately, a scab was forming within the gauze and not over the
incision. So I took off the bandage and let the incision aerate for
four hours, which was enough time for the scab to begin to form.
I got another batch of explanation of benefits forms from my insurance company today, bringing the total cost of treatment over $100,000. As usual, the insurance company misclassified a diagnostic test as "hospital outpatient other" (the blood test was performed in the hospital's outpatient laboratory) and tried to charge me a $50 copay on a $40 blood test. I called the insurance company and they did the usual song and dance about having to look into it and get back to me in a few days. This time they had an additional twist of their computer system having problems.
|
||||
| September 9, 2003 (Tuesday) |
Today is my post-chemotherapy CT scan. My oncologist has ordered a CT
scan of the chest, abdomen and pelvis. Hopefully this will show no
evidence of disease. If it shows any nodes, then I will have to have a
PET scan to distinguish between fibrotic tissue (scar tissue that has
not yet been reabsorbed by the body) and active disease.
The CT scan process was similar to the last time. As before, they told me to drink two containers of the same berry-flavored magic potion and then to change into a hospital gown. The berry shake has to be drunk within a period of ten minutes; I made it with three minutes to spare. Like the last time, I was full to the gills and could barely get the last ounce down. Then I had to wait an hour for the solution to spread through my system. Then they walked me down to the CT, hooked me up to the IV and tossed me through the hole in the doughnut. I could feel the same metallic taste in the back of my mouth, and the hot sensation a bag of popcorn feels just before it pops in the microwave. Like the last time, I asked for a copy of the films. I looked at them when I got home, comparing them to the previous set of films. It looks like the tumors have shrunk, but that there is some residual mass. So I'm guessing that a PET scan will be required. But I won't know for certain until I get a copy of the radiologist's report, as CT scans are difficult to interpret.
|
||||
| September 10, 2003 (Wednesday) |
I got a copy of the radiologist's report on yesterday's CT scan. My May 30, 2003 CT scan showed three tumors in the lymph nodes: a 5 mm tumor adjacent to my heart, a 1 cm tumor just below the diaphragm (in the right retrocrural lymph node), and a 3 cm tumor just above where the aorta splits to go into the legs. The new CT scan shows that the tumor next to my heart is gone. The other two tumors are still present, but have decreased in size. The tumor at the level of the aortic bifurcation has decreased in size from 3 cm to 1 cm. Since there are still nodal masses, a PET scan will be required to determine whether the remaining masses represent active disease or fibrotic tissue (scar tissue that has not yet been absorbed by the body). It is common for seminoma to leave behind fibrotic tissue. The PET scan has not yet been scheduled, as the hospital only schedules them up to four weeks in advance. But hopefully they'll schedule it for four weeks from today. (The PET scan has to be scheduled at least six weeks after my last Neupogen shot, to avoid the possibility of a false negative. My last Neupogen shot was on August 22, and I had a shot of Aranesp on August 25, so the PET scan can be no sooner than October 8.) If the PET scan shows active disease, there are many possible directions treatment can take, including radiation therapy, a RPLND surgery, and further chemotherapy (salvage chemotherapy).
|
||||
| September 11, 2003 (Thursday) |
Some darker facial hairs have started growing, but the bulk of the
facial hair growth is white or translucent. All of the new hair is much
finer than before. My chest hair (what little is left) continues to
fall out.
|
||||
| September 12, 2003 (Friday) |
On Tuesday, September 2, 2003, I was interviewed by CNNfn for a
segment about student financial aid. I wore a suit to the interview,
and decided to take my picture in a mirror before removing the suit.
I do look a little bit like the evil alien from the planet zork in this picture. This was the best of several photographs. The other photographs made me look a little bit like a snearing conehead or a tenctonese "newcomer" without the spots.
|
||||
| September 14, 2003 (Sunday) |
Today was Cancer Survivor Day at PNC Park. A handful of
lectures on cancer topics in the morning were followed by a
Pittsburgh Pirates baseball game in the afternoon.
Finding the venue for the event was a bit confusing. The American Cancer Society provided clear directions on how to get to PNC Park, but didn't specify where the event would be held once one arrived at the park. None of the security guards seemed to know anything about the event either. Eventually I found it by walking all the way around the park. The first talk was about melanoma but very basic. The question and answer session was much more interesting than the talk itself. Next was a motivational speaker who was quite boring and would be a failure at motivating a chicken to cross the road. Most of his talk had something to do with flunking high school and being spanked by his father. The most interesting aspect of the baseball game was the pre-game preparations. First they had six people painting the lines, using a string as a guide. Two of the people carried a six-foot-long paint shield, one used a spray can to paint within the shield, and one held the empty spray cans. I'm not sure what the job of the fifth and sixth people were, but it looked like they were supervising the others. After they were done painting lines, two of the people dragged metal grates on ropes along the dirt to remove scuff marks. The metal grates and rope contraptions looked similar to the tool one uses to create crop circles. I wonder if any of these staff moonlight in corn fields in the midwest? After they were done with this, they used a hose to spray the dirt with water, presumably to keep it from blowing around in the wind. They then reinserted the first through third based into the ground. The game itself was sad. I left after the second inning, when the Pittsburgh Pirates were losing to the Philadelphia Phillies 8 to 0. They tried changing pitchers, but the replacement didn't have any better luck. The fans did give a brief cheer when the Pirates finally got a man on base, but it wasn't very loud, since there were only a few thousand fans present. The price gouging at the ball park was amazing. $3 for a bottle of water, $5.50 for a slice of pizza, $2.50 for a small bag of candy, and $3.50 for a pretzel. Needless to say, I brought my own food. They wouldn't let me take a can of soda into the park, but did let me bring in a bottle of water and a bag of potato chips. I'm not sure I understand the logic, since aluminum is recyclable and Alcoa is based in Pittsburgh. Unfortunately, I discovered that the chemotherapy has made me rather prone to sunburn. After being in the sun for only an hour, my arms and neck had turned bright red.
|
||||
| September 15, 2003 (Monday) |
I asked a friend for some statistics relating to how often the
residual nodal masses left behind by seminoma represent active
disease. He said that Sloan Kettering quotes a 10% rate of active
disease in post-chemotherapy nodal masses, based on pathological
evidence. Indiana University believes the figure is lower, based on a
lower relapse rate. The lower Sloan Kettering figure is probably due
to residual cancer that is in the process of dying. He also noted that
PET scans have been found to be highly accurate with pure seminoma
residuals, with no false positives and very few false negatives. (For
nodal masses smaller than 3 cm, PET scans had a 6% false negative rate
and correctly identified the 9% of seminoma patients where the nodal
masses represented active disease.) So
the odds are that my two remaining nodal masses, which are 1 cm or
smaller, represent fibrotic tissue and that the PET scan should be
able to confirm this.
|
||||
| September 18, 2003 (Thursday) |
I met with my oncologist to review the results of the CT scan. He said
that given the decrease in the size of the tumor masses and my normal
tumor markers, he expects the PET scan to show no evidence of
disease. He's scheduling a CT scan for November 13, representing the
start of surveillance. He will be following a standard surveillance
schedule of every two months during the first year, every four months
during the second and third years, every six months during the fourth
and fifth years, and annually thereafter.
My blood counts were normal, including my red blood cell counts, so there was no need for another shot of Aranesp (Procrit). My veins seem to have recovered, as the nurse had no trouble finding a vein to draw blood. The second wave of facial hair came in dark brown, my normal color. I had a little bit of 5 o'clock shadow today, mostly on my upper lip.
|
||||
| September 22, 2003 (Monday) |
I called the surgeon who removed my gall bladder because the incision
above my belly button was still seeping. He said to not worry about
it, as it takes "months and months" for such incisions to heal
because of the chemotherapy and diabetes. He said to call him in a few
months if it still hasn't healed or if there are signs of infection,
and to keep it covered with a bandaid to soak up the seepage.
|
||||
| September 23, 2003 (Tuesday) |
I had my first physical therapy appointment today, primarily for
evaluation. The physical therapist said that my arms are relatively
weak (they started shaking in the middle of the stretches) and that my
back muscles also needed work. The goal of the physical therapy is to
eliminate the back pain and to rebuild the muscle mass and endurance I
lost during chemotherapy. The physical therapist used electrical
stimulation and heat pads on my back to relax the back muscles. This
was followed by stretches focused on my back muscles and exercises
that addressed my arms, legs and calves. The therapist said I will
need physical therapy two times a week for at least a month. My
appointments will be on Tuesdays and Thursdays.
|
||||
| September 25, 2003 (Thursday) |
During my second physical therapy appointment, the therapist added
three more exercises for my arms.
My eyebrows have started growing back in and are visibly darker. My body hair has also started returning. The hair on the top of my head isn't coming in as quickly, and it looks like the hairs are transparent.
|
||||
| September 29, 2003 (Monday) |
The hair on my head has started growing again. It is coming in
salt and pepper, with more salt than pepper.
|
||||
| October 7, 2003 (Tuesday) |
This physical therapy appointment was similar to the previous one,
except that they added an exercise for the back and use of a
stairmaster. I was only able to last 2.5 minutes on the stairmaster
(9 flights), partly due to fatigue and partly due to pain.
They also added a second set of electrode pads for my shoulder blades in addition to the pads for the base of my back. After a few minutes at an intermediate setting, I quickly became accustomed to the electrical stimulation and ended up at the highest setting.
|
||||
| October 8, 2003 (Wednesday) |
I had my post-chemotherapy PET scan today. I arrived at registration
at 8 am, instead of the scheduled 9 am, because the hospital had
called me the day before to push up the appointment. Apparently
pre-registration had mistakenly scheduled me for the 10th, even though
PET scans are only done on Wednesdays. Since this caused them to be
double-booked for my original time slot, they had to take me earlier.
Since I was one of the first people in the waiting room, there was
hardly any wait for registration this time. (When they're crowded,
there's a waiting time of an hour or more.)
This time they didn't need a catheter. Instead they had me visit the restroom to empty my bladder just before the scan. They said a catheter wasn't necessary this time because my bladder wouldn't obscure the two nodes being questioned by my oncologist. They did a total of six sectional scans. Also, instead of putting in an IV and injecting the radioactive sugar into the IV, they injected the sugar solution more directly. Since I wasn't hooked up to an IV or catheter, I didn't need to change into a hospital gown. As a result, the entire process took about 3 hours or so from start to finish, compared with the 5 hours last time. While I was in the PET scanner, I developed a maddening itch on my face. They not only tell you not to move, but they strap your arms in by your side to prevent you from moving. So I spent 20 minutes trying to not think about the itch next to my nose. It helped that my tush started getting sore, so I could focus on that instead of the itch.
|
||||
| October 9, 2003 (Thursday) |
At my physical therapy appointment today the therapist increased the
number of sets per exercise from 20 to 30 and added two new exercises:
stationary bike (5 minutes) and hand cranks (3 minutes forward and 3
minutes backward). I was very tired afterward.
|
||||
| October 10, 2003 (Friday) |
My oncologist faxed me a copy of my PET scan results today.
The bottom line is "no evidence of FDG avid malignancy".
(FDG is fluorodeoxyglucose, a radioactive sugar. Metabolic activity consumes sugar, causing areas of metabolic activity to show up on the PET scan as hot spots. Many types of cancer, including testicular cancer, show increased metabolic activity. The fact that there were no abnormal hot spots on the PET scan is an indication that the cancer has responded to treatment and is no longer present.) My post-chemo CT scan had shown that the nodal mass adjacent to my heart was no longer present, and that the two abdominal nodes had decreased in size, with the larger of the two decreasing from 3 cm to 1 cm. A PET scan was conducted on Wednesday to determine whether the two residual nodal masses represent active disease or fibrotic (scar) tissue. (Approximately 9% of seminoma cases involving residual nodal masses sized 3 cm or smaller represent active disease.) The PET scan findings were:
The latter is probably referring to the incision above my belly button from the laprascopic gall bladder surgery. In addition, the PET scan noted that "there is interval decrease in FDG uptake within the bone marrow. The bone marrow FDG is within normal limits on the current scan" and "there is no other abnormal FDG activity noted on this scan to suggest the presence of malignancy, with special reference to the retroperitoneum". Since PET scans have a 6% false negative rate when used to stage testicular cancer, this means the probability that I still have active disease is less than 0.5%. The surveillance phase officially begins on Thursday, October 16, 2003.
|
||||
| October 14, 2003 (Tuesday) |
I was very tired after my physical therapy appointment, in part
because the therapist increased the weights and/or doubled the
time. For example, she had me use 9 pound dumbbells with the arm
exercises, and doubled the time on the exercise bike.
I'm still weaker than I was in April, but much better than I was when I first started physical therapy. The back pain is also significantly diminished. She thinks it would be ok for me to join a gym to continue the stretches and exercises on my own, provided my oncologist agrees. She prepared a report for me to take to my oncologist on Thursday. (She did caution me to avoid any abdominal exercises until my belly button incision is fully healed.)
|
||||
| October 15, 2003 (Wednesday) |
It pays to have a copy of your full health insurance
plan document (not the short 2-page summary, but the
100-pager) and to be persistent in appealing claims.
During my last hospitalization, I was admitted to the oncology ward, which has only private rooms. My health insurance policy doesn't cover private rooms, so they wanted to hold me responsible for the difference in cost between a private and a semi-private room. In this case it amounted to a total of $10,196.00 in addition to the $100.00 deductible. My oncologist faxed a letter to the insurance company, indicating that the admission to the oncology ward was medically necessary and that the oncology ward has only private rooms. The insurance company ultimately granted the appeal, because although the health insurance plan normally pays only the average semi-private room rate, there's a clause that states that the plan will pay 90% of the average private room rate if the hospital has only private rooms. The new explanation of benefits form reduces the patient responsibility portion to $982.80 plus the $100.00 deductible. Although $1K still hurts, it is much better than $10K.
|
||||
| October 16, 2003 (Thursday) |
The oncologist appointment went well. My tumor markers are normal (AFP
5.3) and my blood counts are normal (WBC 4.5, Hemaglobin 14.4). (There
was no beta-HCG tumor marker because it was a little less than a month
since the previous beta-HCG last time. There was no LDH tumor marker
because the lab made an error and never tested for LDH even though the
test was ordered.) They drew blood for a fresh set of tumor markers
and will let me know how they turn out.
I'm now officially on surveillance. My first surveillance CT scan will be on November 13, 2003, and I'll have an appointment with my oncologist a week later on November 20, 2003. After that there will be tumor markers and CT scans every two months for the first year, every four months for the second and third years, every six months for the fourth and fifth years, and annually thereafter. My oncologist also said that he's fine with my joining a gym and that it's ok for me to be discharged from physical therapy, so today was my last physical therapy appointment.
|
||||
| October 27, 2003 (Monday) |
The insurance company granted my "special circumstances" appeal
of the remaining $982.80 from my hospitalization in the oncology
ward. So all I have to pay now is the $100 deductible.
|
||||
| November 13, 2003 (Thursday) |
This CT scan wasn't fun. The first attempt at an IV didn't get a good
blood return, and was hurting, so the nurse tried my left arm. This
one got a good blood return, but the vein blew out while the machine
was injecting contrast die, causing about 15 CCs to go into the
muscle. It hurt a lot and caused my biceps to swell up. It looked and
felt like a water balloon. The nurse said
to put it on ice and the swelling and pain should subside by evening.
(It does, however, make one nervous when one hears one nurse telling
the other that she'll have to fill out an incident report.)
The third IV, back in the right arm, worked, and I had the usual metallic taste in the back of my throat. The sense of heat was a bit more intense this time. I felt it in both hands, in addition to my face. I'm guessing that it was more intense due to there being more contrast die in my body this time. I also got a migraine and nausea as a result. I looked at the films from my CT scan, and I can't see any sign of the two residual nodal masses that were present in the previous CT scan. So I'm hopeful that the radiologist's report, which should be available in a few days, will indicate "no evidence of disease".
|
||||
| November 17, 2003 (Monday) |
I just got the CT scan report, and it has some bad news. The
radiologist says that there may be evidence of metastatic disease in
the lower right lobe of the lungs. My oncologist says that it is at
the edge of the resolution of the CT scan, so he wants me to have a
PET scan on Wednesday. The PET scan offers higher resolution and also
indicates whether the nodules are metabollically active or not. Since
my son's surgery is scheduled for Wednesday morning (at a different
hospital), I'm going to try to have the PET scan scheduled for the
afternoon, but I may not have a choice.
I will be meeting with my oncologist on Thursday to go over the PET and CT scan results and to have blood drawn for tumor markers. If the PET and tumor markers are both positive, I'll probably have to have salvage chemotherapy (typically VeIP) and that may start as early as Monday. Or my oncologist may want to wait a month and take another CT scan to see if the nodes grow in size or number. The full radiologist's report is as follows:
Chest: 1. Possible new subpleural nodules posteriorly in the right lower lobe as compared to September 9, 2003. Abdomen: 1. Stable small retrocrural and retroperitoneal lymph nodes. Pelvis: 1. No metastatic disease in the pelvis. COMMENT: CT images were obtained from the lung apex through the symphysis pubis. Oral contrast was given as well as 120 cc of Optiray 320 intravenously. Optiray was used because of a history of diabetes. Comparison is made to September 9, 2003. There are very small subpleural nodular densities seen posteriorly in the right lower lobe which appear new from the prior study of September 9, 2003. They are best seen on image 26. They could represent metastatic disease. No other nodules are seen in the lung parenchyma. There are no enlarged lymph nodes in the hila or mediastinum. No pleural effusion. In the abdomen, there are a few small retrocrural lymph nodes which are stable from the prior examination. The largest of these lymph nodes measures approximately 1 cm in diameter. There is also a residual 1 cm lymph node in the retroperitoneum anterior to the aorta and inferior vena cava. This is also stable. No new adenopathy is seen in the abdomen. There has been prior cholecystectomy. Fatty infiltration of the liver persists. A 1 cm hyperdense focus in the posterior segment of the right lobe of the liver is stable and likely represents a hemangioma. The spleen, pancreas, adrenal glands and kidneys appear normal. No free fluid is seen in the pelvis. In the pelvis, no enlarged lymph nodes or mass is seen. There is no change from the prior examination. Cholecystectomy means surgical removal of the gallbladder. Hemangioma is a benign tumor consisting of a mass of small blood vessels.
|
||||
| November 19, 2003 (Wednesday) |
My son's surgery went well. We got up at 4 am and
arrived at the hospital by 6 am. The Children's
Hospital parking garage does not open until later, so we
had to park in the UPMC garage up the street. After
meeting with the anesthesiologist and a nurse who took
his vitals, we
changed my son into a cute hospital gown and were taken
upstairs to another waiting room, where a
music therapist was playing the guitar and
singing. He went in to the operating room at 7:30 am and
was out about an hour later. He was groggy and
disoriented from the anesthesia, but otherwise doing
very well. We were discharged after
several hours in recovery and post-op. I wanted to drop
my wife and son off at home, but we had to go
straight to the other hospital for my PET scan. Even
though we were discharged with plenty of time to spare,
it took us an hour to get out of the parking garage because
of a traffic jam caused by three buses. I arrived a few
minutes late for the PET scan, but they were waiting
for me.
The PET scan took longer than usual because the machine started scanning in the wrong direction. Instead of scanning from the pelvis to the head, it scanned from the pelvis to the knees. It took two "slices" before I realized that something was wrong. So my full scan ran from my knees to my head. The good news is I don't have cancer in my knees. ;-) Also, my blood sugar level just before the PET scan was 79, which is normal. But that's to be expected, since I didn't eat breakfast or lunch today. The technician let me look at the scans on the computer after the scan was over. There is something on the bottom right lobe of the lung. It could be part of the liver, or it could be part of the lung. If it's part of the lung, it might or might not be cancer. It measures 2.1 mm; 2.5 mm is the threshold for cancer. So it is unclear to me whether I have cancer metastases to the lung or something else. The two most likely candidates for "something else" are Bleomycin-induced pseudonodules or scar tissue, both benign. I'm meeting with my oncologist tomorrow morning, at which time the radiologist's report will be available. After I got home, I realized that it would be helpful to have blood drawn now for tumor markers, so that the results would be available tomorrow to review in conjunction with the PET scan results. I called my oncologist's office and caught them just as they were leaving. They stayed late so that I could rush over and have my blood drawn. (I didn't have to pay for parking during the second trip because it took only 14 minutes from start to finish to have my blood drawn. The parking garage has a 15 minute grace period.)
|
||||
| November 20, 2003 (Thursday) |
Neither the tumor marker results nor the PET scan report were
available when I arrived at my oncologist's office this morning.
My oncologist went over the CT scan with me, pointing out the anomaly identified by the radiologist. He said that based on the location, it was probably not metastatic testicular cancer. If it were lung metastases of testicular cancer, he would have expected it to be in a different location and distributed across both lobes. Then he looked over a PET scan report that had been pulled from the computer, and said that the scan showed no evidence of FDG avid malignancy. He scheduled me for my next CT scan two months from now. I asked for and received a copy of the PET scan report. When I got home I looked at the report and noticed that it was the report from my October PET scan, not the November PET scan. I called the office and the receptionist let the oncologist know that an old report had been pulled from the computer. It turns out that the November PET scan report was not yet available. They promised to call me as soon as they got the PET scan report. I was on pins and needles all day. Around 4 pm I spoke with one of the oncology nurses. They had received my PET scan report and my tumor markers. Both were fine:
The 2.1 mm anomaly I noticed while looking at my PET scan is part of the liver, not the lungs. Coupled with signs of fatty infiltration of the liver and slightly elevated ALT (SGPT) levels, it is most likely related to my diabetes. The full PET scan report is as follows:
Following the IV administration of F18 FDG, a PET scan was performed in transaxial, coronal and saggital images obtained from the skull base to the mid thigh level. Comparison is made to the most recent CT on 11/13/03 and the prior PET student with special attention paid to the right lower lobe where a new subpleural nodule was identified on the CT scan. No abnormal signal is identified within the lungs, specifically the posterior aspect of the right lower lobe where the subpleural nodule was identified on the CT scan. There continues to be moderately increased FDG activity identified in the anterior abdomen superficially, in the subcutaneous tissues close to midline. It is unchanged from the prior study and may represent inflammatory changes. Again clinical correlation is recommended. No other abnormal FDG activity is noted on this scan to suggest the presence of malignancy. IMPRESSION: 1. No evidence of FDG avid malignancy, with special attention paid to the right lower lung zone. 2. Moderate anterior abdominal uptake, superficially. Likely secondary to inflammatory changes with clinical correlation recommended. No change from the prior study. The abdominal uptake is from the belly button incision from my cholecystectomy, which is still healing. The bottom line is my cancer has not relapsed.
|
||||
| November 30, 2003 (Sunday) |
The tinnitus and hearing loss are still present and not
improving. Also, my belly button incision is still not
healing and has become mildly herniated. I've made an
appointment with the surgeon who performed the
cholecystectomy to have him take a look at it.
|
||||
| December 8, 2003 (Monday) |
The doctor who performed the cholecystectomy says that
the incision is not herniated, but instead is showing
some granulation due to an infected stitch. He removed
the stitch and told me to come back in a couple of weeks.
|
||||
| December 14, 2003 (Sunday) |
My tinnitus was worse this entire week because I had a
bad cold. It was extremely distracting and interfered
with anything requiring concentration.
According to the research literature, 20% to 25% of patients receiving cisplatin-based chemotherapy develop tinnitus and high pitch hearing loss that lasts at least two years after the end of treatment. (The hearing loss and tinnitus are bilateral and permanent.) The hearing loss is mostly above the speech range, although a small percentage of patients may experience hearing loss at the higher end of speech frequencies. Total cumulative dosage of cisplatin seems to be the primary risk factor, with about 20% of testicular cancer patients suffering from ototoxicity at standard dosages, increasing to 50% at 400 mg/m2. The severity increases with higher cumulative and higher individual doses. Bleomycin can also cause ototoxicity, to a lesser degree. My hearing loss and tinnitus was caused by the cisplatin during the first week of chemotherapy. There are a lot of snake oil "cures" for tinnitus on the web. None are effective, especially for the tinnitus caused by cisplatin. Current thinking is that the ototoxicity is caused by the loss of cochlear outer hair cells. Practical advice is to avoid making the tinnitus and hearing loss worse. This means avoiding loud noise, caffeine and salt, as well as known ototoxic medications (see ifhoh.org and lhh.org). Some people suggest drinking lots of water can help reduce the severity of the tinnitus.
|
||||
| December 17, 2003 (Wednesday) |
My fingernails have three "waves" corresponding
to each cycle of chemotherapy. The waves are most
apparent in my thumb nails.
The first wave has reached the edge of my fingernail,
and is very brittle. I've torn the edge of two
fingernails perpendicularly and had to trim the nails
back to prevent the tear from spreading.
|
||||
| December 22, 2003 (Monday) |
Today was a follow-up appointment with the surgeon who
performed the cholecystectomy. He removed the scab and
says that the hole has shrunk. There was still some
granulation, but he didn't see any more stitches coming
out. He stuffed the granulation back in where
it belongs and coated the incision with silver nitrate
(stung a bit). He also tested my urine and said I was
negative for glucosuria, meaning that I'm no longer
leaking sugar into my urine. (My before-breakfast blood
glucose level today was 123, and I did not have much
for breakfast. Normal before-breakfast blood glucose
levels are between 80 and 110, so I'm not too far off
from normal.) He told me to come back
in a couple of weeks.
|
||||
| December 30, 2003 (Tuesday) |
Several people have asked me about scholarships for cancer survivors,
since I'm the publisher of FinAid, so I added a new page to
FinAid to provide information about
Cancer Scholarships.
|
||||
| January 5, 2004 (Monday) |
Another follow-up appointment with the surgeon who
performed the cholecystectomy. He removed the scab
and two more stitches, stuffed the granulation back in, and cauterized
the incision and some seepage in the belly button. Since there were a
total of five stitches, that means there's one more stitch that will
probably need to come out.
|
||||
| January 18, 2004 (Sunday) |
I woke up with nausea, vomitting, diarrhea, fever (101.5), headache,
tingling/numbness in the feet and back pain. Since my wife also had
the first four symptoms, I'm assuming that it was a case of food
poisoning. I called the oncologist on call just in case, and he
concurred, but said I should monitor my temperature and call again if
they get worse.
|
||||
| January 19, 2004 (Monday) |
I heard from my urologist today. He was just back from a urology
conference, where he heard about a paper that shows a statistical
correlation between microlithiasis in the contralateral testicle and
carcinoma in situ. Both of my testicles originally showed
microlithiasis. He says that the significance of carcinoma in situ is
unclear (i.e., it isn't clear whether it develops into testicular
cancer), but he thinks it would be wise to have a testicular
ultrasound every six months to monitor for changes in the
microlithiasis. The odds ratio for the contralateral testicle
harboring carcinoma in situ is 28.6 times higher among testicular
cancer patients with contralateral microlithiasis than among
testicular cancer patients without contralateral microlithiasis. Three
quarters of TC patients with contralateral microlithiasis harbored
carcinoma in situ in the contralateral testicle. (The
paper is:
Holm M, Hoei-Hansen CE, Rajpert-De Meyts E, and Skakkebaek NE,
Increased risk of carcinoma in situ in patients with testicular germ cell cancer with ultrasonic microlithiasis in the contralateral testicle.
Journal of Urology 170(4 Pt 1):1163-7, October 2003.)
Another paper, published by Rorth in 2000, indicated that ultimately
all carcinoma in situ transforms into testicular cancer, with 50%
transforming within 5 years and 70% within 7 years.
|
||||
| January 21, 2004 (Wednesday) |
I had my bimonthly CT scan and semi-annual testicular ultrasound of the
contralateral testicle today. I also had blood drawn for tumor
markers. Since I arrived early, they were able to stagger the
radiological exams, performing the ultrasound after I had drunk the
barium sulfate solution but before it had congealed.
The CT scan went well. I had a very good blood return on the first try this time, and no blow outs either.
|
||||
| January 26, 2004 (Monday) |
I met with my urologist today to review the results of the testicular
ultrasound for the contralateral testicle. He said that the ultrasound
was unchanged. There was no evidence of focal parencymal lesion
within the testicle. It still shows the same amount of microlithiasis,
and the small 3 mm epidymal cyst was unchanged in size or
appearance. The size of the testicle itself (4.1 x 2.4 x 3.2 cm) is
normal.
He wants me to have another ultrasound six months from now, in July or August. Essentially, I'm at high risk for carcinoma in situ because of the contralateral microlithiasis, so the best approach is to monitor for contralateral testicular cancer through monthly testicular self exams and semi-annual testicular ultrasounds.
|
||||
| January 29, 2004 (Thursday) |
I met with my oncologist today. The tumor marker results were all
normal, with an AFP of 1.3 ng/mL (normal is 0 to 8) and beta-HCG of <5
(normal is <10). My blood glucose levels were also 94 mg/dL (normal is
currently 65-109, but this will be changing to 65-99 per the November
2003 recommendations from the ADA).
ALT (SGPT) levels continue to be elevated. This time they were 76 (normal is 0-40), up from 64 in November, and 37 in August. This is considered mildly elevated, and is probably related to the diabetes. My CT scans were also fine, showing no signs of metastatic disease or disease progression. The full report is as follows: A routine CT of the chest, abdomen and pelvis was performed, scaning from above the lung apices through the pubic symphysis after the administration of oral contrast and intravenous Optiray. FINDINGS: Comparison is made with previous examination of 11/12/03. CHEST: The lung parenchyma is unremarkable with no definite evidence of pulmonary nodules. There is no airspace disease. No pleural effusions are present. The tracheobronchial tree is intact. There is no mediastinal, hilar or axillary lymphadenopathy. ABDOMEN: The liver is normal in morphology without focal masses or biliary ductal dilatation. There are clips in the gallbladder fossa and the gallbladder has been surgically removed. The pancreas, adrenals, kidneys and spleen are unremarkable. There is no abdominal free air, free fluid or lymphadenopathy. PELVIS: The small and large bowel are normal in caliber without dilatation or obstruction. Again visualized is aortocaval lymph node which is unchanged from the previous examination. No new lymph nodes are identified. There is no evidence of progression of disease. Previously noted left external iliac and small inguinal lymph nodes are stable in appearance. IMPRESSION: 1. CHEST: NO EVIDENCE OF METASTATIC DISEASE. IMPRESSION: 1. ABDOMEN: STABLE ENLARGED AORTOCAVAL LYMPH NODE WITH NO EVIDENCE OF PROGRESSION. IMPRESSION: 1. PELVIS: STABLE LEFT EXTERNAL ILIAC AND COMMON FEMAORAL LYMPH NODES WITH NO EVIDENCE OF DISEASE PROGRESSION. Since my company's new health insurance carrier considers Presbyterian Hospital to be in-network, my oncologist wants me to go there for my next CT scan in two months, to get a PET-CT. A PET-CT scan does both a PET scan and a CT scan simultaneously and can yield additional information, as the two scans complement each other.
|
||||
| January 31, 2004 (Saturday) |
My application for additional life insurance coverage through
my employer was declined by Unum Life Insurance Company of
America. The stated reason was due to my recent history of
testicular cancer. This decision only affects the medically
underwritten portion of my request and does not affect the
coverage for which I was previously approved under my
employer's life insurance plan.
|
||||
| February 16, 2004 (Monday) |
I had another appointment with the surgeon who performed the
cholecystectomy. He was able to grab the last remaining
stitch, but it was so firmly connected that he couldn't pull
up enough of it to cut it. So he used silver nitrate to
cauterize it and said that probably in a month or two the
stitch will come out enough that he can remove it. He said
that a quicker alternative might be to have me come in for
surgery, where he'd make an incision, remove the stitch, and
patch me back up. But we'll wait another month or two before
resorting to that.
I also saw my headache doctor (Dr. Soso). He said if I continue losing weight it should help with the morning headaches, and gave me a prescription for Amerge (naratriptan) for the migraines. He also suggested having my wife use a pulse oximeter to measure my blood oxygenation level when I snore or snort during my sleep. He said to see him again in 18 to 24 months.
|
||||
| February 21, 2004 (Friday) |
My oncologist's office says the insurance will only cover a
CT scan for my next surveillance visit, not a PET-CT. So
instead of going to Presbyterian Hospital for my next
radiological exam, I will go to West Penn Hospital as usual.
|
||||
| February 26, 2004 (Thursday) |
I've been showing some signs of testosterone deficiency, such
as night sweats, diminished libido since the orchiectomy, increased
irritability, and
a persistent decrease in strength despite exercising. I also
sleep more than I did before the orchiectomy, but my mood is
unchanged. A slight difficulty concentrating might be related to this
in addition to the tinnitus. I've also noticed an increased tendency
to make valid word spelling errors (i.e., "principle" vs "principal"),
especially involving context priming of phonologically similar words
(i.e., "child" instead of "college" where "parent" was in the
context). I have also had minor short-term memory lapses, such as
forgetting a number when my concentration is interrupted.
I used the ADAM test (Androgen Deficiency in the Aging Male)
and it indicated a possible testosterone deficiency for me.
During my next meeting with my oncologist I'll
ask him to have my testosterone levels checked.
Long-term potential consequences of low testosterone, besides a reduced risk of prostate cancer, include loss of muscle mass, increase in body fat, and osteoporosis.
|
||||
| March 19, 2004 (Friday) |
The peripheral neuropathy has changed within the last week or
so. Originally, the peripheral neuropathy was a flaring in my hands
and feet. It then changed to a numbness, and then normal sensation
overlayed with numbness. Recently, however, there has been a tingling in my
feet. The tingling is in the front and toes of each foot and on the
outer side (i.e., the right side of the right foot and the left side
of the left foot). It feels sort of like the way a foot does when it
has gone to sleep and is starting to wake up. I feel it all the time
now, but it is more intense after I get up after sitting for a while
(i.e., after sitting during a plane flight). The pads on the thumb,
middle and index fingers of both hands remain numb, although the
middle finger on my left hand has a little more sensation. (That's the
finger I use most often for blood glucose testing.)
My other long-term side effects remain unchanged. I still have the high pitch hearing loss, and the tinnitus is as loud as ever (and louder when I'm in a supine or prone position). I still have occasional nausea. The diabetes has been improving, mostly because I've changed my diet. I still have fatigue and a lack of strength, despite exercising every night (20-40 miles on an exercise bike or stepper, and half an hour with weights for my arms). The belly button incision continues to ooze. (I'm seeing the surgeon again on Monday. Hopefully he'll be able to remove the last remaining stitch. Otherwise I may opt for surgery to remove the stitch.) I got a bill for the January CT scan. It indicates that they have not been paid for the CT scan by my insurance. But my insurance company's web site indicates that they paid the claim. So I'll have to make a few phone calls on Monday to straighten this out.
|
||||
| March 22, 2004 (Monday) |
I had three appointments this morning. The first was with the surgeon
who performed the cholecystectomy. He was able to remove the last
stitch. It hurt a bit, since he had to cut the bottom of the stitch in
order to remove it. But it's out, and that should be the last of the
stitches. I have a followup appointment scheduled for a month from
now, to make sure that the incision is healing over now and not
continuing to drain.
Then I had blood drawn for tumor markers and for checking my testosterone levels. After that, I had a CT scan. It went well. I'm actually getting used to the barium sulfate drink. I was able to drink the two jugs without thinking about how bad it tastes. This time the nurse put the IV into my right forearm. It hurt a little, but it had good blood return. There was the same metallic taste in my mouth and the same hot feeling (must be what food feels like when it is being nuked in a microwave). Afterward, I stayed near a bathroom until the barium sulfate solution decided to flush out the tush.
|
||||
| March 25, 2004 (Thursday) |
I got my blood tests back today. The tumor marker results were all
normal, with an AFP of 2.1 ng/mL (normal is 0 to 8) and beta HCG of <5
mIU/mL. My blood glucose levels were 86 mg/dL (normal is 65-99); I had
not yet eaten that morning.
My testosterone levels were 261 ng/dL (normal for men is 241-827, with most men my age in the 600s). So I'm at the low end of the normal range. However, they didn't check LH, FSH and Prolactin, which are used to determine whether one's body considers the testosterone levels to be normal. If FSH and LH levels are elevated while testosterone levels are low or low normal, that's an indication of a problem with testosterone production in the testis. I've asked my oncologist to check LH, FSH, SHBG and Prolactin levels as well. (Normal levels for Prolactin are 2.1 to 17.7 ng/ml, FSH are 0.9 to 15.0 MIU/ml, and LH are 1.3-12.9 MIU/ml. Normal estradiol levels are less than 54 pg/ml. Of course, what is normal depends on the assay used by the lab; another lab indicates a normal range of 1.4 to 18.1 MIU/ml for FSH.) ALT (SGPT) levels continue to be elevated, but they were lower than January and November. This time they were 57 (normal is 0-40), compared with 76 in January, 64 in November, and 37 in August. This is considered mildly elevated, and is probably related to the diabetes. My white blood cell counts were 7.1 (normal is 4.0-10.5). My red blood cell count was 5.13 (normal is 3.80-5.10). My hemoglobin was 15.3 (normal is 11.5-15.0). My hematocrit was 45.2 (normal is 34.0-44.0). The slight elevation in these counts is nothing to be concerned about. The values would be normal using the reference intervals that were used in January. I was incorrectly listed as female on this report, and I believe they used the wrong intervals for comparison.
|
||||
| March 31, 2004 (Wednesday) |
I used a home cholesterol test kit to measure my total cholesterol. It
indicated that it was 160. If so, that is a significant
improvement. At my next PCP appointment, I'll ask him to do a fasting
lipid profile to double check this result.
|
||||
| April 1, 2004 (Thursday) |
A Pennsylvania insurance broker that specializes in cancer called me
to try to sell me a life insurance policy. Turns out that no insurance
company will insure testicular cancer survivors until they are one
year past the end of treatment. (Most require one to be at least two
years past the end of treatment and symptom-free for the entire
post-treatment period.) At that point it would cost me $4,500
for $500,000 in coverage, taking into account both my cancer and
diabetes. That represents 10-20 times the rates for someone without a
cancer history.
I've heard that insurance rates for testicular cancer survivors at the five year mark (when surveillance appointments drop to one a year) are about four times those for men with no history of cancer. Typically an insurance company will place cancer survivors in their worst rating tier, and also include a surcharge that depends on the number of years since the end of treatment. The surcharge goes away with time, but not the rating. Another possibility is to ask the American Cancer Society (1-800-227-2345) about the high risk pool. Each state has a high risk pool for residents who have difficulty getting insurance. Good articles on this topic can be found at insure.com and smartmoney.com.
|
||||
| April 5, 2004 (Monday) |
My CT scans and tumor markers are all normal. My oncologist has
decided that my CT scans should now be every four months instead
of every two months, so my next CT scan will be scheduled for July.
With regard to the low testosterone issue, although my testosterone was low normal (261 ng/mL), my FSH was 7.7 mIU/mL (1.4 - 18.1 normal), my LH was 2.7 mIU/mL (1.5 - 9.3 normal), and my Prolactin was 3.3 ng/mL (2.1 - 17.7 normal). Since my FSH and LH levels were normal, not elevated, my oncologist says that I am not suffering from testosterone deficiency, per se. He says that it is normal to have lower testosterone with only one testicle, but that my body will gradually adjust and I should give it time.
|
||||
| April 8, 2004 (Thursday) |
I bought a body composition analyzer (a kind of fancy body fat
analyzer, based on electrical impedence). It indicated that I'm
overweight (no surprise, as I'm about 25 pounds heavier than I should
be). My Bone Mass Index was 104 (5.23 lbs), which is normal. My body
water was a little low at 50.6% (88.09 lbs), but I had just exercised.
My body fat was 25.1%, which is 4.1% above ideal. My muscle mass was
92.41 lbs, which is 14.2 lbs below ideal. My basal metabollic rate was
1827 kcal.
I also got a Metrika A1C Now single use home test kit for hemoglobin A1C and used it to measure my hemoglobin A1C. The result was 5.1%, which is normal. A hemoglobin A1C result of 5.1% corresponds with an average blood glucose level of 100-110, which is where I've been for a while.
|
||||
| April 14, 2004 (Wednesday) |
I had a regular doctor's appointment earlier this week. My doctor
had blood drawn for Hemoglobin A1C, Hepatic Function Panel, and Lipid
Panel. My Hemoglobin A1C was 5.5%, a little higher than the home test
kit, but still excellent. My cholesterol was 216 (normal is under
200), HDL was 52 (normal is over 40, but over 60 is desirable), LDL
was 141 (normal is under 130), Cholesterol/HDL was 4.2 (normal is
under 5.0), and triglicerides was 114 (normal is under 150).
Even though this is an improvement over the previous levels, my doctor
wants me to start taking Zocor and baby aspirin.
The hepatic function panel was all normal. In particular, my ALT levels were 29, which is far better than the levels reported by my oncologist two weeks before. Albumin was 5.1 (normal is 3.7 to 5.1). My doctor wants to start me on Zocor and baby aspirin. I want to confirm the cholesterol results first. (I ran another home cholesterol test today and it came back with total cholesterol 168, so I'm wondering about the accuracy of the higher results.) My doctor prescribed ketoconazole shampoo for some dermatitis just above my eyebrows. This dermatitis started during my chemotherapy, but had recently gotten worse. I had never had any dermatitus or eczema before.
|
||||
| April 19, 2004 (Monday) |
The surgeon examined the drainage site in my belly button, and said
that it is about 95% healed. He scheduled a follow-up appointment for
two months from now, when it should be 100% healed.
|
||||
| April 21, 2004 (Wednesday) |
I spoke with my PCP. He agrees that rather than take Zocor right now,
I should continue with the weight loss and see if I can't resolve the
high cholesterol through diet and exercise. After I've lost another 20
pounds, if my cholesterol levels are still high, then we'll consider
taking Zocor (and maybe niacin too). I will be getting a Cardiochek
cholesterol monitor to monitor my cholesterol levels every month or
so. The Cardiochek monitor has test strips to check total cholesterol,
HDL and triglycerides. LDL figures can then be derived through
calculation using the Friedewald formula: Total Cholesterol = LDL + HDL +
(fasting triglycerides/5).
When trying to control Cholesterol levels through diet, one should aim to eat less saturated fat and more unsaturated fat. Dietary cholesterol comes mainly from meat, poultry, fish and dairy products. Vegetables and fruit contain no cholesterol. Other dieting tips can be found in a UMass newsletter. HealthLink has a calculator for estimating an LDL cholesterol goal.
|
||||
| April 28, 2004 (Wednesday) |
This evening, while I was in Chicago, my eyes started itching and
burning. It was incredibly painful, and the whites of my eyes were
completely red. I took some antihistamines and it cleared it up.
Before the cancer, I would only get itchy eyes when I
mowed the lawn, and the allergic reaction was never bad enough that I
needed to take something for it. I wonder if this allergic reaction is
somehow related to the chemotherapy?
|
||||
| May 7, 2004 (Friday) |
My Cardiochek monitor arrived yesterday, so this morning I ran a
fasting lipid test. My total cholesterol was 200, HDL 56,
Triglycerides 94, and LDL (calculated) 125. Cholesterol/HDL was 3.6. I
ran the test twice. The second time total cholesterol was 209, HDL 52,
Triglycerides 96 and LDL 138.
I had another allergic reaction today, this time in Pittsburgh while walking the dogs. I took some antihistamines to solve the problem.
|
||||
| May 10, 2004 (Monday) |
I had another allergic reaction today, again in Pittsburgh while
walking the dogs in the park. I took some more antihistamines and it solved the
problem, but I'm reluctant to return to the park because the reaction
was so severe.
|
||||
| July 6, 2004 (Tuesday) |
I had a CT scan and semi-annual ultrasound today, as well as a blood
draw for tumor markers.
The hospital had a new type of barium sulfate oral contrast solution called CheeTah, but it tasted about the same as the previous oral contrast drink. The first CT nurse had trouble finding a vein, hitting a tendon twice and a nerve once, and so a different nurse took over and took two tries to find a vein. It was probably due to inexperience, since the nurse at my oncologist's office took only one try to draw blood. But I did end up being a pincushion today. I took at brief look at the ultrasound films, and they looked ok -- uniform gray except for white specs due to the microlithiasis. The ultrasound tech also examined the fossa to make sure that everything there was ok.
|
||||
| July 9, 2004 (Friday) |
Another wisdom tooth bit the dust as a casualty of the
chemotherapy. When the upper wisdom tooth crumbled because of
chemotherapy, it chipped off part of the lower wisdom tooth. I didn't
think much of it, since it seemed to still be functional. But during a
recent dentist appointment my dentist said there was a hole in the
tooth and that it should come out.
Today an oral surgeon extracted the tooth. He had to give me four shots of novocaine because I was still sensitive, but after the fourth shot I didn't feel a thing. (After the first two shots the numbness extended to the corner of my mouth, but my tongue was not at all number. The third shot brought the fuzziness to the midline of my face, but the tongue side of my gums was still sensitive. The fourth shot made everything numb. The oral surgeon said that I must have atypical nerve anatomy, or particularly sensitive nerves.) After that, the tooth came out quite easily, even though it was a lower wisdom tooth. A few wiggles with the right tool, and it popped right out. This was much easier than the removal of the upper wisdom tooth last year. The oral surgeon had very good bedside manner and was thorough and careful. He was meticulous in reviewing the informed consent form with me, and had my blood pressure, pulse, and blood oxygenation level monitored automatically throughout the extraction. I was impressed. Dr. Wible even called me at home five hours after the procedure to see how I was doing -- to check whether the bleeding had stopped, whether the pain medication was working, and whether I had any questions. So now I have only two wisdom teeth left. Two wisdom teeth and one testicle.
|
||||
| July 14, 2004 (Wednesday) |
I met with my urologist today. He received copies of the reports for
both the ultrasound and CT scans, and said that everything is fine. He
gave me a script for fertility testing (semen analysis) since I'm
about a year after the end of chemotherapy.
My urologist is moving his office to Butler, Pennsylvania, about an hour away. Since I only need to see him twice a year, I'll continue with him as my urologist. He will no longer have privileges at West Penn Hospital, so if I need surgery I'll have to switch urologists. But if surgery is necessary, I can switch to a different urologist at that time. The text of the ultrasound report is as follows: INDICATION: Left microlithiasis, history of seminoma in the right testis, status post right orchiectomy. FINDINGS: Testicular ultrasound was performed. Comparison is made with previous study of 1/21/04. The right testis has been removed and there are no remarkable findings in the right testicular fossa. The left testis measures 4.3 x 2.3 x 2.2 cm. Tiny punctate echogenic foci are present throughout the testis consistent with microlithiasis. No focal nodules are identified. There has been no significant change from the previous study. The left epididymis is unremarkable with the exception of a tiny epididymal cyst in the head. A small amount of fluid is present in the scrotal sac. IMPRESSION: 1. A LEFT TESTICULAR MICROLITHIASIS WITH NO EVIDENCE OF AN INTRATESTICULAR MASS, NOT SIGNIFICANTLY CHANGED FROM 1/21/04. 2. TINY EPIDIDYMAL HEAD CYST. The text of the CT scan report is as follows: CLINICAL HISTORY: Testicular carcinoma. Comparison 3/22/04. The patient received nonionic contrast due to diabetes history. FINDINGS CHEST: The lungs are clear. No pleural or pericardial effusions. No adenopathy or nodules. There is a mild amount of residual thymic tissue in the anterior mediastinum. FINDINGS ABDOMEN: The liver, pancreas, spleen, adrenal glands and kidneys are unremarkable. The gall bladder has been removed. FINDINGS PELVIS: A tiny aortocaval lymph node as well as a left external iliac lymph node are stable. These are subcentimeter in size. Benign appearing small inguinal nodes are stable. The patient has had right orchiectomy. No suspicious osseous lesions. A sclerotic focus likely representing a bone islands, in the left iliac bone is stable. IMPRESSION CHEST: 1. NO EVIDENCE FOR DISEASE. IMPRESSION ABDOMEN: 1. NO EVIDENCE FOR DISEASE. IMPRESSION PELVIS: 1. STABLE SUBCENTIMETER AORTOCAVAL AND LEFT EXTERNAL ILIAC LYMPH NODES.
|
||||
| July 16, 2004 (Friday) |
This morning I went to the local cryobank for semen
analysis (fertility testing), as almost a year has
passed since the end of chemotherapy. I should get the
results back sometime next week. My understanding is
that chemotherapy doesn't affect the ability of sperm to
create a viable embryo, but that if the chemotherapy
does have the potential to cause infertility by halting
sperm production. So if there are any sperm in the
sample, even at subfertile levels, they can potentially
improve with time as my body recovers from the
chemotherapy. But if there are no sperm in the sample,
then the infertility is permanent.
|
||||
| July 19, 2004 (Monday) |
The semen analysis showed a subfertile result of 16
million sperm per ml. Anything above 20 million is
considered fertile.
On June 13, 2003, before chemotherapy, the cryopreservation results showed a concentration of 45 million sperm per ml. A subfertile result does not mean that a pregnancy cannot be achieved, just that it may be less likely or may require artificial insemination. All other sperm paramters were normal, including forward progression, activity, round cells and agglutination.
|
||||
| July 26, 2004 (Monday) |
One last stitch appears to be coming out through the
drainage site in my belly button. So far it isn't
infected, so I'm going to let it come out on its own.
If it doesn't make any progress over the next few
weeks, or gets infected, I will make an appointment with
the surgeon to have it removed.
|
||||
| July 29, 2004 (Thursday) |
I had a routine surveillance appointment with my
oncologist today. My oncologist's practice has moved
into a new building, consolidating several
locations. The building is very nice and shiny.
Everything was fine. As noted previously, my CT scan and ultrasound showed everything stable, with no signs of malignancy. My beta HCG was normal, as was my CBC. My next appointment is in approximately 4 months, and will be scheduled for a week after my next CT scan.
|
||||
| August 11, 2004 (Wednesday) |
Today I had a quarterly doctor appointment with my PCP for diabetes
management. He said I look fine, and that I've lost 11 pounds since
the previous appointment. He had blood drawn for hemoglobin A1C and
thyroid.
|
||||
| August 17, 2004 (Tuesday) |
I just got a copy of the lab report from my recent doctor
appointment. My Hemoglobin A1C was 5.2%, a good value.
My TSH was 1.27 mU/L (normal is 0.40 to 5.50 for my age and sex) and my T4,FREE was 1.2 ng/dl (normal is 0.8 to 1.8 for my age). So I have normal thyroid function.
|
||||
| November 8, 2004 (Monday) |
I had another CT scan today, along with a blood draw. I arrived at the
hospital early, hoping that they'd be able to squeeze me in early, but
they apparently got me confused with another patient and I ended up
being scanned half an hour after my original appointment.
The receptionist, a nice little old lady, was no longer there. She apparently retired a few months ago. But the new receptionist was nice too, and handed me my usual two bottles of oral contrast. This time the nurse was able to insert the IV the first time without problems. I had the usual metallic taste, but this time the sense of heat was confined to my right side. My hand felt particularly hot. I think they scanned my kidneys and liver an extra time. I held my breath and didn't move, so I don't think it was because the images were blurry. After the CT scan I drove to my oncologist's new office to have my blood drawn for tumor markers. The phlebotomist was at lunch (the delay in my CT appointment had spilled over into lunchtime), so I had to wait 40 minutes. Again the nurse was able to hit the vein the first time without problems. However, she shifted the needle after filling two vials and was not able to recapture the vein. Rather than stick me a second time, she transferred some blood from one vial to a third for use with the CBC, since she had enough blood.
|
||||
| November 12, 2004 (Friday) |
The appointment with my oncologist went well. My tumor markers remain
normal, with beta HCG under 5 and AFP of 1.6. My CT scan report was
also good, showing no change. After the next four-month appointment,
if everything remains fine he wants to switch me to a six-month
schedule.
The text of the CT scan report is as follows: CT CHEST/ABDOMEN/PELVIS 11/8/04 HISTORY: Testicular cancer. Comparison to prior study of 7/6/04. A routine CT of the chest, abdomen and pelvis was performed, scanning from above the lung apices through the pubic symphysis after the administration of oral contrast and intravenous Optiray. CHEST: There is no intrathoracic adenopathy. No pleural or pericardial fluid is noted. The lungs are clear. IMPRESSION: 1. NO EVIDENCE OF METASTATIC DISEASE IN THE CHEST. ABDOMEN: The liver, spleen, pnacreas, adrenals and kidneys are normal. The gallbladder has been removed. Small aortic caval lymph node measuring approximately 5 mm in short axis is unchanged from previous study. No enlarged lymphadenopathy is noted. IMPRESSION: 1. NO EVIDENCE OF METASTATIC DISEASE IN THE ABDOMEN. PELVIS: There is no evidence of bowel obstruction or bowel wall thickening. Small left external iliac lymph node is unchanged from previous study. No new lymphadenopathy is identified. IMPRESSION: 1. STABLE SMALL LEFT EXTERNAL ILIAC SUBCENTIMETER LYMPH NODE WITH NO EVIDENCE OF NEW LYMPHADENOPATHY.
|
||||
| December 15, 2004 (Wednesday) |
Today I had a quarterly appointment with my PCP to follow-up on my
diabetes. He said that my diabetes is so well controlled by diet and
exercise that we can reduce the frequency of the visits to twice a
year. My hemoglobin A1C was 5.0%, in the non-diabetic range. My total
cholesterol was 188, HDL 54, LDL 119, and triglicerides 74, with a 3.5
ratio of total cholesterol to HDL. So my cholesterol has also
normalized through diet and exercise. Losing 50 pounds did the trick.
|
||||
| January 6, 2005 (Thursday) |
Another semi-annual testicular ultrasound. This is the first time one
of my ultrasounds didn't coincide with a CT scan. The tech did the
scans, with the usual measurements of the epidymal cyst and one or two
other small densities. The testicle as a whole had the usual uniform
gray with white specs from the microlithiasis.
|
||||
| January 13, 2005 (Thursday) |
This morning I saw the surgeon who performed the cholecystectomy a
year and a half ago. I reported that my drainage site was still
occasionally draining and bleeding, but no signs of an infection. This
time, however, I could see the tail of a stitch poking out of the
drainage site. The surgeon was able to grab it, cut the loop of the
stitch, and remove it. Since that was the sixth stitch (he says that
it is unusual for him to use more than five), this should be the end
of it. He says that I shouldn't need to see him again, since the
drainage site should now be able to heal properly.
|
||||
| January 18, 2005 (Tuesday) |
I met with my urologist today for a semi-annual exam and to review the
ultrasound. Everything was fine. He says that because my father has
rising PSA scores, it might be a good idea for me to have my PSA score
taken to establish a baseline. He also said that we should continue
with semi-annual ultrasounds until I reach the three year mark, and
then we'll switch to annual.
The text of the ultrasound report is as follows:
SCROTAL SONOGRAM 1/6/05 CLINICAL HISTORY: 37 year old male with testicular seminoma status post right sided orchiectomy. COMMENT: Realtime and color Doppler ultrasound of the scrotum was performed. Comparison is made to the previous study done on 11/8/04. The left testis is visualized. There is microlithiasis present. No focal masses are present within the left testis. The left testis is homogeneous, with the exception of the microlithiasis. There is a small epididymal head cyst or spermatocele measuring 4 x 3 x 4 mm. There is a small hydrocele on the left. No testis is identified on the right due to the patient's surgical resection. There is good flow to the left testis. IMPRESSION: 1. LEFT TESTICULAR MICROLITHIASIS WITHOUT FOCAL MASS PRESENT. RECOMMEND YEARLY FOLLOW UP. 2. STATUS POST RIGHT SIDED ORCHIECTOMY.
|
||||
| March 14, 2005 (Monday) |
I saw my oncologist today to review the results of my CT scans and
tumor markers.
My tumor markers were all normal. My AFP was 1 ng/mL and my beta HCG was < 5 mIU/mL. He also performed a CBC, with the following values: WBC 4.8, RBC 4.95, HGB 14.6, HCT 44.3, MCV 89.4, MCH 29.4, MCHC 32.9, Platelet 259, all normal. My other blood chemistry values were also normal. In particular, my ALT was 18 U/L, in the middle of the normal range. The text of my CT scan report is as follows: A routine CT of the chest, abdomen and pelvis was performed, scanning from above the lung apices through the pubic symphysis after the administration of oral contrast and intravenous Optiray. Comparison 11/08/04. FINDINGS: CHEST - There are a few small retrocrural lymph nodes, the largest measures 1 cm short axis, not significantly changed. There is no lymphadenopathy in the chest. No pulmonary nodules, pleural or pericardial effusions seen. ABDOMEN - The liver, spleen, pancreas, both adrenal glands, and both kidneys are normal in appearance. Cholecystectomy clips noted. No retroperitoneal lymph nodes greater than 1 cm; the retroperitoneum is stable in appearance. PELVIS - The appearance of the pelvis is unchanged. The subcentimeter left external iliac lymph node described previously is stable. The bowel is unremarkable. There is a well defined sclerotic lesion in the left iliac bone which is unchanged. CHEST IMPRESSION: 1. NO EVIDENCE OF INTERVAL METASTATIC DISEASE. ABDOMEN IMPRESSION: 1. NO EVIDENCE OF INTERVAL METASTATIC DISEASE. PELVIS IMPRESSION: 1. NO EVIDENCE OF INTERVAL METASTATIC DISEASE. My next CT scan will be scheduled for six months from now. Because I was experiencing severe Raynaud's phenomenon at the time of the appointment (my hands were bright red and my fingers were visibly swollen), my oncologist ordered additional blood tests to make sure it wasn't unrelated to the chemo. Depending on the test results, he'll refer me to a rheumatologist. He is also having my PSA levels checked to establish a baseline, because my father was diagnosed with prostate cancer last month.
|
||||
| April 18, 2005 (Tuesday) |
My new primary care physician tested my blood glucose levels at 93 and
my hemoglobin A1C at 5.7, both in the non-diabetic range. My
microalbumin was also normal.
|
||||
| July 26, 2005 (Tuesday) |
My urologist said that the ultrasound showed no changes. There is no
change in the microlithiasis, nor in the epididymal cyst. He conducted
a clinical testicular exam, and said that everything is fine.
Because my father was diagnosed with prostate cancer and my last prostate exam was two years ago, he conducted a prostate exam. He said that everything is fine, and that I have the prostate of someone half my age. He will check with my oncologist about the PSA test results, and if the PSA test wasn't done, will schedule an annual PSA test for me. He believes that we should continue with ultrasounds at the same frequency as my CT scans, but offset by a few months. My next ultrasound will be in six months.
|
||||
| August 11, 2005 (Thursday) |
My urologist called my oncologist to obtain my PSA levels from my
March 14 exam, and reports that they were 0.22. Anything less than 2
is normal for my age, so this was an excellent result.
|
||||
| September 7, 2005 (Wednesday) |
I had my semi-annual CT scan today. My oncologist had scheduled the CT
scan for the same hospital, so that I would be scanned using the same
equipment and have my scans read by the same radiologist. However,
West Penn Hospital just replaced all of their CT scan equipment with
new Toshiba 64-slice CT scanners. These scanners have 16 times the
resolution of the conventional 4-slice CT scanners they used
previously.
A conventional CT scan has a slice thickness of 8 mm to 10 mm. A high resolution CT (helical CT, spiral CT, HRCT) has a slice thickness of 1 mm to 1.3 mm and can image about 40 slices simultaneously. The Aquilion has a slice thickness of 0.5 mm (with contrast) and can image 64 slices simultaneously. Without contrast the resolution is 2 mm. They still gave me oral and IV contrast for my scan, and they still had the "hold your breath" announcement during the scan, although the scan ran much more quickly (about 10 times faster). They also changed the procedure a bit; instead of having the IV inserted while I was on the scan table, they had it inserted in advance. (I guess they are trying to schedule the use of the equipment more efficiently. Given that the scans are quicker, more of the time is taken up by inserting the IV. By pipelining the IV insertion, they are able to schedule more scans per hour. The radiology waiting room was fuller than before.) A common problem with high resolution CT scans is the higher resolution doesn't always increase the accuracy. Often the higher resolution means the CT scan detects more artefacts that ultimately turn out to be benign. It will be interesting to see if the even higher resolution of the Aquilion CT scan results in even more false positives. (The technician commented that they are often using the new CT scanner to resolve questions that arise from the use of their PET-CT scanner.)
|
||||
| September 19, 2005 (Monday) |
I met with my oncologist today. He reported that my tumor markers and
CT scan results were both normal, no sign of cancer. He suggested that
I should see an endocrinologist, partly because of the diabetes and
partly because of the low testosterone. (The CT scan did have an
incidental finding of gynecomastia.)
The AFP levels were 2 ng/mL (normal is 0-6) and the beta HCG was <2 mIU/mL (normal is 0-9). The text of my CT scan report is as follows: INDICATIONS: Testicular cancer. A routine CT of the chest, abdomen and pelvis was performed, scanning from above the lung apices through the pubic symphysis after the administration of oral contrast and intravenous Optiray. Comparison is made to 3/7/05. FINDINGS: CHEST: The lungs appear clear. There are no pulmonary nodules. There are no pleural or pericardial effusions. There is no suspicious adenopathy within the chest. Incidental note is made of gynecomastia. IMPRESSION: 1. NO EVIDENCE OF METASTATIC DISEASE TO THE CHEST. ABDOMEN: Cholecystectomy clips are noted in the right upper quadrant. The liver, spleen, bilateral adrenal glands and kidneys appear normal. The pancreas appears normal without evidence of pancreatic ductal dilatation. There is no suspicious adenopathy within the abdomen. IMPRESSION: 1. NO EVIDENCE OF METASTATIC DISEASE TO THE ABDOMEN. PELVIS: The large and small bowel appear normal. There are no inflammatory changes or fluid collections in the pelvis. There is no abnormal adenopathy in the pelvis. The right testicle and right spermatic cord are surgically absent. IMPRESSION: 1. PELVIS: NO EVIDENCE OF METASTATIC DISEASE OR DISEASE RECURRENCE.
|
||||
| November 17, 2005 (Thursday) |
I saw my endocrinologist today for the first time. She confirmed the
gynecomastia, but said that it was fairly mild (i.e., very little
breast tissue). She's ordering a pretty full workup: comprehensive
metabolic panel, lipid panel, c-peptide, FSH/LH, Hemoglobin A1C,
Prolactin, Testosterone (Free), Testosterone (Total), TSH, T4 (Free),
microalbumin/protein/creatinine ratio, estradiol, Quant HCG, and AFP.
|
||||
| December 22, 2005 (Thursday) |
I had my semi-annual ultrasound today. Since the radiologist was out
for the holidays, they will not be able to give me the films until
next week.
|
||||
| December 29, 2005 (Thursday) |
I picked up the ultrasound images today. Instead of giving me films,
they gave me a CD-ROM with both the current images and the images from
June.
The December ultrasound shows the epididymal cyst to measure 0.28 cm by 0.28 cm by 0.36 cm. The June ultrasound shows the epididymal cyst to measure 0.27 cm by 0.26 cm by 0.32 cm. The difference in size is not significant. In both cases this would be reported as a 3 mm by 3 mm by 3-4 mm cyst. The December ultrasound also shows the testicle as measuring 2.30 cm by 4.92 cm by 3.24 cm, compared with the June ultrasound measurements of 2.42 cm by 4.72 cm by 3.25 cm. The differences are insignificant. Both ultrasounds show similar levels of microlithiasis and uniform density. I believe that the radiologist's report will indicate no change and no sign of malignancy.
|
||||
| January 31, 2006 (Tuesday) |
I saw my urologist today. The ultrasounds were normal: no sign of
malignancy, the microlithiasis is unchanged in amount and
distribution, and the epididymal cyst is unchanged in size. My PSA was
0.22, unchanged, and an excellent result.
I also heard from my endocrinologist that my total testosterone was 255 ng/dL, free testosterone 60.1 pg/mL (normal 35.0 - 155.0), and that my estradiol was 13 pg/mL (normal 10-50). FSH was 4.7 mIU/mL (normal 1.0 - 18.0), AFP was 1.7 (normal < 6.1), beta-HCG was <1, Prolactin 5.0 ng/mL, and LH was 4.1 mIU/mL. The percent free testosterone was 2.36% (normal 1.0% - 3.1%). All values are within the normal range, although the testosterone is at the low end of normal. TSH was 1.43 (normal 0.35 - 5.50) and Free T4 was 1.2 (normal 0.9 - 1.8). Other results from my endocrinologist include blood glucose of 117 mg/dL (normal is 75 to 100) and hemoglobin A1C of 6.0 (normal 4.8 - 6.0). Cholesterol was elevated at 236 mg/dL (normal 10-199) with triglycerides of 121 and HDL of 57 and LDL (calculated) of 155. ALT (SGPT) was 77, above the normal range of 30-65. C-Peptide was 3.1 (normal 0.8 - 3.1).
|
||||
| February 13, 2006 (Monday) |
I had my semi-annual CT scan and tumor markers blood draw today.
There is something worse than berry-flavored barium sulfate solution. It is pina-colada-flavored barium sulfate solution. The stuff tasted so bad I wanted to vomit, and the rest of the day my bowels were complaining.
|
||||
| February 20, 2006 (Monday) |
I met with my oncologist for my semi-annual appointment. My tumor
markers were normal (AFP 2 ng/mL, beta HCG < 2 mIU/mL). My CBC was
normal: WBC 6.6, RBC 5.27, HGB 15.2, HCT 46.9, MCV 89.0, MCH 28.8,
MCHC 32.4, and Platelets 275.
The 2/13/06 CT scan also showed no sign of metastatic cancer:
Technique: A routine CT of the chest, abdomen and pelvis was performed, scanning from above the lung apices through the pubic symphysis after the administration of oral contrast and intravenous Optiray. Indication: Testicular cancer. Comparison: 09/07/05. Chest Findings: The lungs appear clear without evidence of pulmonary nodule. There are no pleural or pericardial effusions. There is no suspicious lymphadenopathy within the chest. The bones and soft tissues appear normal. IMPRESSION: CHEST: 1. NO EVIDENCE OF METASTATIC DISEASE IN THE CHEST. Abdomen Findings: The liver, spleen, bilateral adrenal glands and kidneys appear normal. Within the tail of the pancreas there is a 1 cm increased attenuation nodule which appears stable compared to previous study. Cholecystectomy clips are present within the right upper quadrant. There is no suspicious lymphadenopathy within the abdomen. IMPRESSION: ABDOMEN: 1. NO EVIDENCE OF METASTATIC DISEASE TO THE ABDOMEN. Pelvis Findings: There are no abnormally enlarged lymph nodes within the pelvis. There is a well-defined sclerotic lesion in the left iliac bone, which is also stable in appearance. There are no abnormally dilated loops of small or large bowel. There are no inflammatory changes or fluid collections within the pelvis. The right testicle and spermatic cord are surgically absent. IMPRESSION: PELVIS: 1. NO EVIDENCE OF METASTATIC DISEASE OR DISEASE RECURRENCE IN THE PELVIS. We also discussed my Raynaud's Phenomenon and occasional mild back/hip pain. The back pain is unlikely to be related to the cancer, since it is symmetric and mild and the onset was long after the end of chemotherapy (i.e., no possibility of femoral head necrosis). He offered to order a lower back MRI if the back pain got worse. He also gave me the name of a rheumatologist for the Raynaud's.
|
||||
| August 7, 2006 (Monday) |
I had my semi-annual CT scan today. The barium sulfate solution tasted
a bit sour and was harder to get down than usual. The nurse was new
and had trouble starting an IV. She tried five times (including twice
hitting a nerve) before giving up and letting another nurse do it. The
more experienced nurse took two tries. She first tried in my forearm,
but that one wouldn't flush. She then kept talking about how fat and
puffy a vein on the back of my hand was, until I relented and allowed
her to use it. Of course, she went through a nerve to hit the vein;
the veins on my hands are right next to the nerves. (At my oncologist's office
later that day, the phlebotomist took only one try to get blood for
tumor markers. But then again, it is a thinner gauge needle.) So I
ended up looking like a pincushion, with a half dozen pieces of white
gauze taped over my wounds.
The barium sulfate solution didn't sit very well with me. I had extremely loud bowel sounds and had to stay near a bathroom for the rest of the day. I also felt a bit nauseous from it. I wonder if it had somehow 'turned'.
|
||||
| August 8, 2006 (Tuesday) |
I had my semi-annual ultrasound today. When I showed up for my
appointment they had me preregistered, but not appointment was
scheduled. Apparently they had moved the ultrasound room since I made
the appointment and forgot to move the appointment, so I was scheduled
for a nonexistent room. I had to wait 1.5 hours while they squeezed me
into the schedule. Then I walked over to the new facility, where they
temporarily had lost my paperwork. Other than that, the ultrasound was
fine.
The testicle is a uniform gray with the amount of microlithiasis apparently unchanged. The testicle measured 2.16 cm by 4.82 cm by 3.25 cm, compared with the December measurements of 2.30 cm by 4.92 cm by 3.24 cm. The slight decrease in size is within the realm of operator variability. The epididymal cyst measures 0.07 cm by 0.10 cm by 0.13 cm, which is definitely smaller than before.
|
||||
| August 14, 2006 (Monday) |
I met with my oncologist today. My CT scans and tumor markers are all
normal. We will continue with the semi-annual surveillance schedule
until I reach the 5-year mark.
My CBC from August 7, 2006 was as follows: WBC 7.2, RBC 5.25, HGB 15.7, HCT 46.9, MCV 89.4, MCH 29.9, MCHC 33.5, Platelet 275, all normal. My tumor markers were Beta HCG < 2 mIU/mL (0-9 is normal) using the Bayer Centaur/ACS methodology, and AFP 2 ng/mL (0-6 is normal) using the DPC Immulite methodology. The text of the CT scan report was as follows: TECHNIQUE: A routine CT of the chest, abdomen and pelvis was performed, scanning from above the lung apices through the pubic symphysis after the administration of oral contrast and intravenous Optiray. CLINICAL HISTORY: Testicular carcinoma follow-up examination. COMPARISON: 02/13/06 CHEST FINDINGS: There is no mediastinal or hilar lymphadenopathy. The lung parenchyma is normal in appearance. No pericardial or pleural effusion seen. ABDOMEN FINDINGS: There is diffuse fatty infiltration of the liver. No focal lesions or biliary dilatation. The spleen, pancreas, both adrenal glands and both kidneys are normal in appearance. There is no retroperitoneal lymphadenopathy and no ascites is seen. PELVIS FINDINGS: No pelvis lymphadenopathy. Sclerotic lesions left iliac crest is stable, likely a bone island. IMPRESSION: CHEST: 1. NO EVIDENCE OF INTERVAL METASTATIC DISEASE. ABDOMEN: 1. DIFFUSE FATTY INFILTRATION. 2. NO EVIDENCE OF METASTATIC DISEASE. PELVIS: 1. NO EVIDENCE OF METASTATIC DISEASE.
|
||||
| August 15, 2006 (Tuesday) |
The appointment with my urologist was routine, a dip strip test of a
urine sample, a review of the
ultrasound results followed by a clinical testicular exam. Everything
is fine.
The text of the ultrasound report was as follows: CLINICAL HISTORY: Follow-up microlithiasis, left testicle. FINDINGS: The right testicle is surgically absent. There has been no change in the microcalcifications in the left testicle. No mass is seen in the left testicle. A small amount of fluid is seen around the testicle. The left epididymis shows normal size. There is again noted a small cyst in the epididymal head, measuring 2 mm on the current study. A left varicocele is demonstrated. IMPRESSION: 1. No change in the microlithiasis of the left testicle. 2. Small amount of fluid around the left testicle. 3. No evidence of lest testicular mass. 4. Right testicle is surgically absent.
|
||||
| January 2, 2007 (Tuesday) |
I met with my oncologist today to review the results of my tumor
markers and CT scans from December 21, 2006.
The tumor markers showed beta hcg less than 2 mIU/mL and AFP of 2 ng/mL, both normal. The CT scan showed no sign of metastatic cancer in the chest, abdomen and pelvis. However, the CT scan shows a 1 cm mass in the tail of the pancreas that is consistent with a nonfunctional neuroendocrine tumor. A review of the original staging CT scan from 5/30/03 shows the tumor unchanged. It is surprising that the radiologists did not notice this sooner (I've had 12 CT scans before this), especially given the history of pancreatitis and gall stones. Given this finding and my history of pancreatitis, gall stones, and diabetes, my oncologist scheduled an MRI of the pancreas for Thursday. If the mass is confirmed as a nonfunctional neuroendocrine tumor of the pancreas, likely treatment will involve surgical resection. Five year survival for this form of pancreatic cancer is 50%. However, mine is small and apparently indolent, and there does not appear to be any metastasis, so the odds are possibly more favorable. My CBC was mostly normal, with AST elevated at 39 U/L (normal is 5-34), ALT elevated at 65 U/L (normal is 10-40), and blood glucose elevated at 120 mg/dL (normal is 70-105). The text of the CT scan report is as follows: 12/21/06 CT CHEST, ABDOMEN AND PELVIS ENHANCED The following is the interpretation of the teaching physician whose signature is below: INDICATION: Testicular cancer. COMPARISON: CT chest, abdomen and pelvis from 8/7/06 and 5/30/03 A routine CT of the chest, abdomen and pelvis was performed, scanning from above the lung apices through the pubic symphysis after the administration of oral contrast and intravenous Optiray. FINDINGS: CHEST: The lungs are clear with no pleural effusion or pneumothorax. There is no abnomal lymphadenopathy within the chest. There is no pericardial effusion. The heart and intrathoracic aorta are normal in appearance. Osseous structures of the chest are also normal in appearance. ABDOMEN: There is diffuse, fatty infiltration of the liver. There has been prior cholecystectomy. The spleen, adrenal glands and kidneys are normal in appearance. There is a 1 cm hypervascular mass in the tail of the pancreas which is likely consistent with a nonfunctioning neuroendocrine tumor. In retrospect, this lesion appears unchanged as compared to study from 5/30/03. There is no abnormal lymphadenopathy or fluid collection in the abdomen. PELVIS: Multiple loops of bowel are normal in caliber with no evidence of wall thickening or obstruction. There is no abnormal lymphadenopathy within the pelvis. There are no pelvic fluid collections. There is stable, well circumscribed sclerotic lesion of the left iliac bone which is likely on the basis of a bone island and is unchanged from prior study. Bones are otherwise normal in appearance. IMPRESSIONS: CHEST: 1. NO EVIDENCE OF METASTATIC DISEASE TO THE CHEST. ABDOMEN: 1. A 1 CM HYPERVASCULAR LESION WITHIN THE TAIL OF THE PANCREAS, LIKELY CONSISTENT WITH NONFUNCTIONING NEUROENDOCRINE TUMOR. THIS IS STABLE IN APPEARANCE SINCE 5/30/03. 2. FATTY LIVER. 3. NO EVIDENCE OF METASTATIC DISEASE WITHIN THE ABDOMEN. PELVIS: 1. NO EVIDENCE OF METASTATIC DISEASE WITHIN THE PELVIS.
|
||||
| January 4, 2007 (Thursday) |
I had an MRI of the pancreas today (along with bits of the liver of
spleen).
This was the first time I had an MRI. After completing a questionnaire about previous surgeries and numerous questions that all asked whether there was any metal in my body (answer: just some clips from prior surgeries), they repeated the questions in an interview just to be sure. I then changed into hospital pants (regular pants have too much metal in the zipper and snap) and put all my belongings into a locker, including anything with metal (keys, cell phone, rings, watch). The machine looks pretty much like the doughnut they use for a CT scan or PET scan, although the doughnut hole is a little snugger fit. They had a nice 3x3 grid of ceiling tiles that looked like blue skies with fluffy clouds to stare at before they slid you into the MRI. They felt for the bottom of my rib cage and the top of my pelvis for positioning, and had me skootch back an inch so that everything was lined up. They inserted the IV for the IV contrast in my right arm, taping it in several places so that it wouldn't move, and coiled the tube around by thumb twice (and taped it down as well). They placed a 'coil' on my chest to help focus and transmit the MRI information and strapped it down, turning me into a turtle. Before sliding me into the MRI, they put earphones on my head (tuned to an oldies/country music station) and a panic squeeze bob in my left hand. The sound quality on the earphones was pretty bad, but it helped dull the shrieking/banging sound of the MRI as it fired up. They also delivered the "take a deep breath" and "hold your breath" instructions through the earphones, although sometimes I missed the first part and had to breathe in in a hurry. They had me hold my breath for 30-60 seconds, which was stretching it with the coil on my chest. One time I think they forgot to tell me to breathe again. The IV contrast felt cool as it slid up my arm (if I had synethesia, I'd say it felt like silver of mercury), but turned hot as soon as I felt the metallic taste in the back of my mouth. The MRI was very loud, making a "braaaaaack" sound that varied a little in pitch and speed, and my nose itched the entire time. My shoulder was stiff by the time they were done.
|
||||
| January 10, 2007 (Wednesday) |
I had a frustrating wait to hear the results of my MRI. The report was
faxed to my oncologist on January 5, but his patient load was high
enough that he didn't get around to reading charts until January 10.
The text of the MRI report is as follows:
I found a reference that indicates that resection of localized primary
tumor has a 5-year survival rate of 72% with a median survival of 6.8
years. (See Douglas B. Evans, et al, Nonfunctioning islet cell
carcinoma of the pancreas, Fourteenth Annual Meeting of the American
Association of Endocrine Surgeons, Williamsburg, VA, April 25-27,
1993.) This compares with the overall 50% five-year survival figures
reported by other researchers.
|
||||
| January 15, 2007 (Monday) |
I dropped by my oncologist's office for some bloodwork. They drew
blood to test for Chromogranin A (CgA), a marker for neuroendocrine
tumors of the pancreas. They also gave me a container for 24-hour
collection of urine for 5-HIAA testing.
I'm supposed to avoid eating bananas, avocados, plums, eggplant, tomatoes, plantain, pineapples and walnuts for a 72 hour period before and during collection (i.e., for 48 hours before and throughout the collection period). The collection starts in the morning, with the first urination of the day discarded (and the time marked). All subsequent urinations are collected and transferred to the collection container until the next morning. The collection container must be refrigerated. My wife wrinkled her nose when I told her I'd be storing urine in the refrigerator.
|
||||
| January 26, 2007 (Friday) |
My Chromogranin A test came back 4 (normal). The 5-HIAA test came back
as 5.5 (normal is 0 to 8.0).
|
||||
| February 19, 2007 (Monday) |
I had my semi-annual urologist appointment today. The testicular
ultrasound of the contralateral testicle showed stable microlithiasis
with no sign of cancer. The urologist also gave me a clinical
testicular exam, which was normal.
Total testosterone was 193 (normal is 250-1100), so I'm now officially testosterone deficient. However, free testosterone was 2.55 percent (normal is 1.0 to 3.1) and my FSH and LH were normal. Since I'm asymptomatic of testosterone deficiency and have a family history of prostate cancer, my urologist prefers to hold off on testosterone replacement therapy until it is clearly necessary. If I were to ask him for TRT he would prescribe it, but right now I'm comfortable with monitoring the testosterone levels (T Total and T Free, FSH and LH) on an annual basis. At my next semi-annual appointment I'll ask him about getting a bone scan to establish a baseline. My PSA was 0.2 (excellent) and unchanged from a year ago. My prostate exam was normal ("the prostate of a man half my age"). My SGPT was 77, which is a little high (65 is the upper end of normal). The text of the ultrasound report is as follows: CLINICAL HISTORY: History of right testicular carcinoma. Follow up for left microlithiasis. FINDINGS: The scrotal contents were scanned and the transverse and longitudinal plans. The right testis has been resected. The left testis measures 4.6 cm x 2.6 cm x 2.8 cm. It contains numerous small calcifications. A left epididymal head cyst measures 0.2 cm x 0.2 cm x 0.2 cm. A left hydrocele and a left varicocele are present. In the previous examination of 8/8/2006, the left epididymal head cyst measured 0.1 cm. The varicocele and hydrocele were present at that time. IMPRESSION: 1. STABLE LEFT MICROLITHIASIS. NEGATIVE FOR AN INTRATESTICULAR MASS. NEGATIVE INTRATESTICULAR DOPPLER INTERROGATION. 2. SMALL LEFT EPIDIDYMAL HEAD CYST. 3. LEFT HYDROCELE. 4. LEFT VARICOCELE. 5. RIGHT ORCHIECTOMY.
|
||||
| March 9, 2007 (Friday) |
I thought I was having a PET scan today, but it turns out that my
oncologist had ordered a PET-CT scan. That explains why it took so
long for the insurance company to approve it. It was in the same
trailer as was used for my PET scan in 2003, but with a new Siemen's
Biograph 8 PET-CT scanner.
Getting to the hospital was a little roundabout. The 31st street bridge has been closed for a while for repairs, so normally I take the 16th street bridge. But I heard on the radio that there had been an accident on Liberty Avenue between 16th and 17th streets (apparently a 16 year old girl had been struck and killed by a car), and the police had shut down Liberty Avenue in both directions. So I had to drive all the way into Shadyside to approach the hospital from the south instead of the north. This made me arrive 10 minutes late for registration, but that didn't cause any problems. My oncologist's office told me to show up on the third floor radiology. They should have sent me to the basement MRI department. But the ladies in radiology were able to register me and send me down to the basement. I was escorted onto a platform lift on the side of the trailer (I guess they don't trust patients to walk up the stairs). Inside the trailer it was air conditioned despite an ambient temperature of 45 degrees outside. First the nurse checked my blood sugar. She said it was 190, which is strange, since I checked it myself that morning and it was much lower. Given that I was fasting for the test, it should not have increased. In any event, it was below the 200 threshold. The nurse was able to insert the IV in my left arm with just one poke. As with a PET scan, they inject you with mildly radioactive sugar (5-HTP). This time was a little different than the last time. This time involved an interesting syringe filled with saline. They first checked that I had good blood return, then screwed the metal cannister containing the radioactive sugar onto the side, and pulled back on the syringe before pushing in the plunger the inject the sugar. I guess it must have a one-way valve. After 45 minutes they escorted me to a bathroom to empty my bladder, and then returned me to the trailer. I waited another 5 minutes before they were ready to scan me. There were some nice improvements in the process. First, they had form-fitting pillows for my head and under my knees, so it was much more comfortable. When I raised my hands over my head as instructed, I found that the pillows even had indentations for my hands. They also didn't need to strap me into a cocoon, because the test was much quicker. The PET-CT has 8 detectors instead of 4, cutting the time in half. First they ran two quick passes for the CT scan portion, then one very slow pass with seven "segments" for the PET scan. The technician said that my oncologist would receive the report Monday or Tuesday. He had already blanked the screen, so I couldn't sneak a peak at the scan.
|
||||
| March 12, 2007 (Monday) |
I saw the gastroenterologist, Dr. Richard Kim, today. He will schedule
me for an endoscopic ultrasound (EUS) with biopsy.
He says this is the only definitive way of determining
whether the 1 cm mass is neuroendocrine tumor of the
pancreas, fibrotic tissue, or something else.
The endoscopic ultrasound is an outpatient procedure. They spray the back of the throat with a local anesthetic to block the gap reflex, and then administer a sedative. First a regular scope goes down the throat to look around, then it is replaced with the EUS scope. They will look at the pancreas through the wall of the stomach and take a needle biopsy. Normally Dr. Kim would do the EUS himself, but his facility does not have the capability of taking a biopsy (EUS-FNA). So he will be scheduling me for the EUS with Dr. Dhawan at Allegheny General Hospital. Dr. Kim's office was interesting. Instead of the usual aquarium of tropical or salt water fish, it has an aviary. The aviary was built by Living Design Inc., a company that builds aviaries for doctor's offices. This aviary had two doves, a canary, and eleven finches.
|
||||
| March 17, 2007 (Saturday) |
I received a copy of the report from Dr. Richard Kim, the
gastroenterologist. I was impressed by the thoroughness and his
automatically sending me a copy of the report without my needing to
ask for it.
The text of the report is as follows:
Reason for Visit: Pancreatic mass. History of Present Illness: Mark is a 39-year-old male seen in consultation at Dr. Barsouk's request for evaluation of a pancreatic lesion. Mark has a history of stage III seminoma treated with chemotherapy and is now felt to be free of disease. He was noted to have a one cm hyperechoic lesion at the tail of the pancreas dating back as far as 2003. A recent CT scan confirmed this finding and has been unchanged. He did undergo an MRI of the pancreas as well and it confirms the presence of the lesion 16 mm from the tip of the tail of the pancreas. He really has no symptoms. There are no episodes of pain. He has no clinical episodes of pancreatitis. He has no systemic symptoms. He denies any flushing. He denies any change in his weight. His seminoma is essentially cured. Past Medical History: 1) Stage III seminoam eradicated with chemotherapy; 2) Migraine headaches; 3) Status post cholecystectomy with ERCP; 4) Orchiectomy; 5) Appendectomy. Medications: Amerge for migraines. Allergies: Zofran. Health Habits: Denies cigarette or alcohol abuse. Family History: Heart disease, hypertension, non-colon cancer in a father. Heart disease and non-colon cancer in grandparents. Review of Systems: GENERAL - Recent weight gain, night sweats. EYES - No visual disturbances. ENT - Ringing in the ears, bleeding gums, frequent sore throats. CARDIOVASC - No exertional chest pain. RESP - No exertional dyspnea, wheezing, hemoptysis, productive or persistent cough. GU - No hematuria or dysuria. MUSCULAR - No muscle weakness. SKELETAL - No persistent joint pain. SKIN - No persistent rash. NEURO - Migraine headaches. PSYCH - No history of significant mental disturbance. ENDOCR - No history of hormonal disorder. HEME - Treated for testicular cancer. Physical Examination: He is a pleasant, well-developed male in no apparent distress. Height: _'_''. Weight: 194 lbs. BP: 124/74. Heart rate: 76. Temperature: 97.8. Respirations: 16. Skin - no rashes, petechiae, purpura, or palpable masses. Eyes without scleral icterus. Conjunctivae are pink. Lids normal. PERLA. Posterior pharynx is normal without erythema. Neck is supple without masses, or thyromegaly. Lungs are clear to auscultation and percussion. Cardiac exam is regular rate and rhythm without murmurs, gallops or rubs. Abdomen exam is normal, active bowel sounds, soft, nontender, nondistended. No hepatosplenomegaly. No masses. Extremities - no clubbing, cynanosis, or edema. Lymphatic - no palpable cervical, or inguinal lymphadenopathy. Psychiatic - alert and oriented x 3. Memory grossly intact. Diagnostic Data: As per the HPI. Impression: 1. Hyperechoic lesion in the tail of the pancreas which has not changed in size in the last 3 years. I suspect this is either going to be a non-functioning neuro endocrine tumor. Alternately, it could have been a metastases from the seminoma but this would certainly be somewhat unlikely. I think we should evaluate further with an endoscope. This probably needs to be biopsied as well under endoscopic ultrasound guidance. I did tell him that while we do diagnostic endoscopic ultrasounds in our center, in order to get a fine needle aspiration though at the same time, this would have to be done in Allegheny General Hospital or UPMC. His insurance covers Allegheny General Hospital; therefore will refer him to Dr. Dhawan for an EUS FNA of the pancreatic mass.
|
||||
| March 19, 2007 (Monday) |
I got a copy of the report from my PET-CT scan of March 9, 2007. It
shows no sign of FDG avid malignancy. This means that if the 1 cm mass
at the tail of the pancreas is metastasis from the testicular cancer,
it is almost certainly fibrotic tissue (scar tissue) and not active
cancer. This does not, however, rule out the possibility of
nonfunctioning neuroendocrine tumor of the pancreas, as such tumors
are often not FDG avid. So I still need to have the EUS-FNA.
The text of the PET-CT report is as follows: INDICATION AND HISTORY: 39-year-old male for restaging testicular cancer. RADIOPHARMACEUTICAL: F-18 FDG 14.2 mCi IV. Blood glucose at the time of injection was 190 mg/dl. TECHNIQUE: FDG PET and CT scans were obtained from the skull to the proximal mid thights. CT scans were obtained without oral or intravenous contrast for the purposes of attenuation, localization and image fusion. FDG PET scans were reviewed with and without attenuation correction and CT fusion. COMPARISON: PET scan 11/19/2003 FINDINGS: There are no hypermetabolic foci seen in the head and neck, chest, abdomen and pelvis to suggest FDG avid malignancy. The previously noted hypermetabolism in the anterior abdominal wall is not seen on the current study. There is no hypermetabolism seen in the region of the tail of the pancreas corresponding to the hypervascular lesion seen on prior CT scan. IMPRESSION: 1. NO HYPERMETABOLIC FOCI TO SUGGEST FDG AVID MALIGNANCY.
|
||||
| April 2, 2007 (Monday) |
Since I hadn't received a call from Allegheny General Hospital to
schedule the EUS-FNA, I called the doctor's office and the nurse who
handles the scheduling said that they
had never received my medical records. So I called the
gastroenterologist and spoke with the nurse who was supposed to send
my records. She faxed the records today, and I got a call back from
the scheduling nurse. My EUS-FNA is scheduled for May 14, 2007 (the
earliest available date). It's the usual deal: bloodwork 1-2 weeks
prior, nothing to eat or drink after midnight, must be driven to/from
the procedure as I can't drive for 24 hours afterwards due to the
aftereffects of anesthesia, and must arrive at the hospital at least
1.5 hours before to prep for the procedure. The actual procedure
itself lasts 30-45 minutes, followed by 45 minutes or so waking up
from anesthesia. I'll probably end up with a sore throat.
|
||||
| May 1, 2007 (Tuesday) |
I had a blood test (platelets) in preparation for the upcoming
biopsy. The phlebotomist hit the vein for the first vial, but then
shifted the needle losing the vein. After fishing around for the vein
for a while (pretty painful), she gave up and tried the other arm. No
luck there either. Third time was successful, but it was also a pretty
painful stick. I got the feeling that maybe she was a little
inexperienced at blood draws.
|
||||
| May 14, 2007 (Monday) |
I had my endoscopic ultrasound and fine needle aspiration biopsy
(EUS-FNA) today. I should get the results in about a week.
Getting to the hospital was pretty easy. We took 279 south to the East Street Exit (8b), turned right on North Avenue and right again on James Street. The garage was packed, so we ended up parking on the roof. Luckily it was a sunny day. We took the elevator to floor 1 (hospital level). The nurse who had called me earlier with directions said that it had a yellow star next to the one, but she was incorrect. We then took a maze of twisty little passages, walked down the hisotry hall and ended up in the main lobby with registration on the right. Registration was interesting. After the receptionist took my information, she handed me one of those pager/coasters they use in restaurants. We wandered over to the gift shop and browsed for a while before sitting in the chairs. A few minutes latter it buzzed and we were ushered into registration. Since I was preregistered it was mainly a matter of providing my insurance card, giving some medical history (allergies, previous surgeries) and getting two wrist bands (one for identification and one for allergies). We then took the elevator to floor "01" (the floor below "1") and turned right to the "GI Lab". We were about an hour early, but only had to wait 20 minutes before the admitting nurse could see me. She took a more detailed history and showed me into the GI lab, where I changed into a gown from the waist up. I then got on a gurney and a nurse (Cynthia) installed an IV with a saline drip. They let me continue wearing my glasses until the procedure. I was parked next to a supply cabinet, so I got to watch the nurses come and go as they prepped other patients. The anesthesia doctor and nurse dropped by with the usual questions. They told me that instead of a general anesthesia they were going to give me a strong sedative which would keep me awake and breathing without intubation. They assured me that afterward I wouldn't remember a thing. Dr. Dhawan then dropped by to explain the procedure and obtain consent. He said that the scope has a water-filled balloon at the end, which they press against the side of the stomache and use to look at the pancreas with ultrasound. If they can localize the mass, they then use a fine needle through the wall of the stomach to take tissue samples for a biopsy. The usual risks (perforation, bleeding) are minimal. They then wheeled me over to the scope room, where I was hooked up to a three-lead EKG, pluse oximeter and pressure cuff. They also inserted a bit guide in my mouth to protect my teeth from the scope and to protect the scope from my teeth. They had me roll over onto my left side and that's the last thing I remember until waking up in recovery. I woke up with a sore throat and a tummy ache (presumably from where they took the biopsy). The nurse gave me a choice of apple juice, cranberry juice or ice water. I took the latter. My wife came by to keep me company while the cobwebs dissolved. She also rubbed my neck where I had developed a stiff neck from lying on my side. After half an hour a nurse came by to disconnect the pressure cuff, pulseox and EKG and to remove the IV (taking some hair with it). I then changed back into my clothes and we waited for Dr. Dhawan to come by to say how it all went. He said that the preliminary slides showed no sign of cancer (meaning adenocarcinoma of the pancreas) but that further study/staining would determine whether it is islet cell tumor (i.e., neuroendocrine tumor of the pancreas) or completely benign. He said that there was no sign of metastasis; the lymph nodes were all clear. He said that if it was islet cell tumor, the surgery is pretty straightforward given the location at the tail of the pancreas. After another short wait, the discharge nurse came by with the discharge instructions, warned me not to sign any contracts for the next day, and then chided me when I tried signing the discharge instructions (my wife was supposed to sign).
|
||||
| May 18, 2007 (Friday) |
I got a copy of the reports from my endoscopic ultrasound (EUS) and
fine needle aspiration biopsy (FNA) today. The nurse said that she had
never seen a biopsy report that referred to acinar cells. The doctor
had already left for the day, so I won't hear his interpretation until
Monday.
The reports seem to be ruling out both fibrotic tissue and non-functioning neuroendocrine tumor of the pancreas. The latter is part of the endocrine system, and acinar cells are part of the exocrine system. The new possibilities now under consideration are normal pancreatic tissue and pancreatic acinar cell carcinoma (PACC). The latter is very rare and difficult to diagnose. Best guess is that I will need further testing before my gastroenterologist can recommend appropriate management of the mass. Or he may just say that it should be surgically removed.
EUS: Indications: Nonspecific abnormal findings on radiological and other examination of gastrointestinal tract. Asymptomatic pt with recent CT that showed tail mass, similar in size to CT from 2003. Procedure: The procedure, indications, preparation and potential complications were explained to the patient, who indicated his understanding and signed the corresponding consent forms. The phsyical exam was performed. The patient was administered CS-ANES anesthesia. Supplemental oxygen was used. The patient was placed in the left lateral decubitus position and an endoscope was introduced through the mouth and advanced under direct visualization until the third part of the duodenum was reached. Careful visualization of the upper GI tract was performed. The procedure was not difficult. The patient tolerated the procedure well. There were no complications. Findings on the upper endoscopy: Esophagus: Normal esophagus Stomach: Normal stomach Duodenum: Normal duodenum Additional notes: EUS: Normal pancreas seen throughout except for a hypoechoic lesion seen in tail of pancreas measuring 11 mm by 9 mm. No peri-pancreatic abnormalities noted. Under doppler guidance, 4 passes made with 25 G FNA needle and specimen submitted for analysis. IMPRESSION: Pancreatic tail mass; likely non-functioning islet cell tumor. FNA CYTOLOGY (NON-GYN) REPORT: FINAL DIAGNOSIS TAIL OF PANCREAS MASS, FINE NEEDLE ASPIRATION AND CELL BLOCK: 1. ACINAR CELLS ARE PRESENT (SEE COMMENT) 2. FURTHER STUDIES ARE RECOMMENDED. Note: The aspirate is moderately cellular with monotonous cells. The cell show abundant granular amphophilic cytoplasm, round nuclei with occasional nucleoli. Immunostaining panel was performed and the cells are negative for NSE, synaptophysin, chromogranin, MAP-2 and positive for alpha1 antitrypsin and alpha1 chemotrypsin. This pattern confirms that these cells are acinar in origin. No atypia or mitosis is seen. Acinar cells can be seen in benign pancreatic tissue and also in acinic cell carcinomas. Also, two groups of ductal cells with mild-moderate atypia can be identified. Further diagnostic studies and/or tissue confirmation is recommended if clinically indicated.
|
||||
| May 31, 2007 (Thursday) |
I got a call from my gastroenterologist to discuss the endoscopic
ultrasound and fine needle aspiration biopsy (EUS-FNA). He said that
although the tissue was mostly normal pancreatic tissue, there were a
few atypical cells that appear to be precancerous. Specifically, there
were two groups of ductal cells with mild to moderate atypia. It does
not seem to be islet cell tumor. This is
not a definitive diagnosis. It could be normal pancreatic tissue, or
it could be precancerous acinar cell carcinoma. There were no
peripancreatic abnormalities noted (i.e., no signs of metastasis).
My gastroenterologist is recommending surgical resection via a distal pancreatectomy. He feels that it is most likely a precancerous lesion and that further testing (i.e., more biopsies) is unlikely to yield a definitive diagnosis. Since the mass is located at the tail of the pancreas, surgical removal is simpler than if it had been located at the head of the pancreas and there are unlikely to be long-term consequences of the surgery. Given this, and my young age, he feels that surgical removal is the wisest course of action. I had independently sent copies of my pathology reports to a national expert on pancreatic cancer who also recommended surgical removal. He said that pancreatic masses generally don't realize malignant potential until they are at least 2 cm in size, and that it is best to remove it when it is small before it has a chance to metastasize. Curiously, he still thinks that it is probable that this is a nonfunctioning neuroendocrine tumor of the pancreas since it is often difficult for pathologists to distinguish acinar cells from neuroendocrine cells. My gastroenterologist's nurse called his colleagues at other local hospitals to help find an experienced surgeon who is in-network for my insurance at an in-network hospital. She found a surgeon who specializes in laparoscopic liver surgery (150+ cases) and also has significant experience with pancreatic surgery. A family friend who is a doctor at the local cancer institute thinks very highly of his surgical skills, referring to him as a "magician and super star with his hands". I am scheduled to meet with him on Wednesday, June 13, 2007.
|
||||
| June 13, 2007 (Wednesday) |
I met with a surgeon at UPMC Passavant hospital this morning. He says
that I can definitely have a laparoscopic distal pancreatectomy and
that they may even be able to do a laparoscopic enucleation. The
latter is like a lumpectomy. With a distal pancreatectomy there's a
chance they might need to remove the spleen; that's avoided with an
enucleation. He will meet with the surgeon who would be actually doing
the procedure later today to review the MRI scans to get a better
sense of whether an enucleation is possible.
The hospital stay after the procedure would be 2 days, and one week recovery at home (no driving, minimal exertion, but I could use a laptop to work). I might return home with drains that would need to be removed later. This is much better than an open procedure, which would require 2 weeks in the hospital and 2 months recovery at home. They've done a series of 80 laparoscopic distal pancreatectomies. This is probably the longest such series in the US. (Other groups may have done more distal pancreatectomies, but not laparoscopically.) They had 1 mortality (1.25%), an elderly woman who died of a heart attack two weeks after the surgery. The main complication is fistulas (fluid leaks) which usually resolve on their own. In some cases they've had to perform an ERCP to install a stent to release the pressure to enable the fistula to close on its own. I will be meeting with a surgeon at West Penn Hospital next Thursday. This surgeon is in the same practice as the surgeon who performed my laparoscopic cholecystectomy. He's ordered a dedicated pancreatic CT scan, which will give a good look at the pancreas and surrounding blood vessels and organs. This will be useful for either surgeon, regardless of who I choose.
|
||||
| June 21, 2007 (Thursday) |
I went to West Penn Hospital this morning. First I had a
"dedicated CT scan of the pancreas". Then I met with the surgeon.
The dedicated scan of the pancreas was similar to other CT scans I've had, except it was just of the upper abdomen. I had to drink only one bottle of oral contrast, instead of two. They also injected the IV contrast much quicker, causing my hands, throat and tush to feel like they were burning up. The results were a mixed bag. The surgeon consulted with the radiologist about the scan, and said that it showed two lesions on the pancreas, not just the one at the tail of the pancreas. The second lesion was about 1.5 cm and on the body of the pancreas. They compared it with one of my 2004 CT scans and found the second lesion there as well. So even after they realized they had missed the first lesion on my original CT scans, they still missed the second one. Amazing! The CT scans are being reviewed by the head of radiology. So if I need surgery, this means a much more complicated procedure which will involve removing much more of the pancreas. The long term consequences of such surgery are also more severe. However, the surgeon said that he thinks it would be more appropriate to monitor the lesions than to surgically resect them. He doesn't think that it is acinar cell carcinoma. If it was, I should have been dead two years ago. He also said that he doesn't think it is neuroendocrine tumor. He also says that it looks like the lesions may have shrunk by a few millimeters of the past four years. But he can't say what the lesions are. They aren't due to inflammation from the pancreatitis I had the second week of chemotherapy, because they were present before I had the pancreatitis. But he raised the possibility that the atypical cells were caused by the pancreatitis, even if the lesions themselves weren't. He's ordered a bunch of blood tests to rule out acinar cell carcinoma. So now I have one surgeon and my gastroenterologist saying that I need surgery, and another surgeon saying that I don't. They will consult with each other to try to resolve the differences. I will probably need additional tests, such as a biopsy of the second pancreatic mass, and will probably ask for a second opinion on the pathology from a major center for pancreatic surgery, such as Johns Hopkins or Sloan Kettering. Issues I want resolved include:
I will wait until I receive a copy of the CT scan report to instigate getting these issues resolved. I want all of my doctors to consult with each other until they reach agreement as to the appropriate management of my case. I'm concerned that the doctors aren't going to be able to provide a definitive diagnosis.
|
||||
| June 27, 2007 (Wednesday) |
I received a copy of my CT scan and blood test results today.
The blood tests showed amylase of 33 (normal 30-110 U/L) and lipase of 30 (normal 6-75 U/L). If I had acinar cell carcinoma one would expect both of these to be elevated. ALT (SGPT) was 50 (normal 21-72 U/L) and AST (SGOT) was 28 (normal 17-59 U/L). Sodium and chloride were a little low, but not significantly so. Blood glucose was elevated. The text of the CT scan report is as follows: CT ABDOMEN UNENHANCED, ENHANCED JUN 21, 2007 8:20:00 AM TECHNIQUE: Unenhanced CT of the abdomen was performed followed by imaging in the pancreatic parenchymal and portal venous phases during rapid injection of 125 cc Optiray-320 intravenous contrast. HISTORY: Pancreatic mass, followup COMPARISON: 12/21/2006 and multiple prior CT exams back to 2003. FINDINGS: There is marked diffuse fatty infiltration of the liver. There are 2, slightly hyperdense and mildly hypervascular lesions in the pancreas, one in the pancreatic body measures 1.5 cm and is seen best on more delayed images (7-107). Compared to multiple prior studies the lesion is not significantly changed. The 1 cm lesion in the pancreatic tail is also stable. The remainder the pancreas normal. The adrenal glands, spleen both kidneys and bowel are normal in appearance. There is no retroperitoneal lymphadenopathy. There is no ascites. IMPRESSION: 1. Two hypervascular lesions in the pancreas which are stable over multiple exams likely represent nonfunctioning islet cell tumors 2. Diffuse fatty infiltration of the liver
|
||||
| July 2, 2007 (Monday) |
I met with the pancreatic surgeon who specializes in laparoscopic
surgery today. He's done more than 100 laparoscopic distal
pancreatectomies.
He said that there are two main options for dealing with the two pancreatic masses:
An enucleation is probably not possible due to the location of the masses. The surgeon recommends against it because of the greater likelihood of fistulas (leakage). It is a difficult decision. If I go with surveillance and it turns out to be cancer, there's a chance it will metastasize between scans. Surgery is only curative before metastasis. Nothing is curative after metastasis. On the other hand, if I go with surgery and it turns out to be benign, I will have had surgery with the negative consequences mentioned above. There is insufficient information to provide a definitive diagnosis, and there likely won't be even with further tests. The surgeon did suggest that there's a possibility that the biopsy missed the mass at the tail of the pancreas and instead hit normal tissue. Plus, the original EUS-FNA did not biopsy the mass in the body of the pancreas. A second biopsy might yield a more definitive diagnosis. It's kind of weird to be wishing for a cancer diagnosis, but I'm more uncomfortable with the lack of a definitive diagnosis than the possibility of a cancer diagnosis. Next steps are as follows:
|
||||
| July 3, 2007 (Tuesday) |
My gastroenterologist's office called today. They are going to order a
second EUS-FNA at Allegheny General Hospital. I will be called after
the holiday to schedule it.
|
||||
| July 19, 2007 (Thursday) |
The surgeon who performed my first EUS-FNA biopsy called me today to
discuss my case. He said that he had examined the entire pancreas from
head to tail during the first ultrasound and did not see the body
lesion, just the tail lesion. But it is there on the CT scan.
He also says that the tail mass is unusual. If it were just normal pancreatic tissue, as the biopsy suggested (aside from two groups of atypical ductal cells), it should not be showing up on the ultrasound as a mass and the CT scan as hyperdense and hypervascular. Acinar cell carcinoma was subsequently ruled out by normal amylase and lipase (plus acinar cell carcinoma is aggressive and would not go dormant for four years). In light of the unexamined body mass and the inconclusive results from the first biopsy, he concurs with my gastroenterologist and the other two surgeons. He is recommending a second EUS-FNA to examine and biopsy both masses. He will do multiple passes on the two masses to make sure that there enough cells are gathered to allow for a second opinion from Johns Hopkins or Sloan Kettering, if necessary. I have agreed, and his scheduling nurse will call me to schedule a date for the procedure. It will likely be sometime in August. Like the previous one, this will be an outpatient procedure under general anesthesia. My intuition is that the first biopsy missed the tail mass and hit normal pancreatic tissue. I believe that the most likely diagnosis is nonfunctioning neuroendocrine tumor of the pancreas. (It would be most consistent with certain nonspecific symptoms, such as frequent headaches and the need for frequent bathroom breaks.)
|
||||
| July 24, 2007 (Tuesday) |
I had my semi-annual ultrasound today. The amount and distribution of
microlithiasis appears
unchanged and the testicle otherwise has a uniform gray appearance (no
focal densities). The epididymus measures 1.03 cm by 1.29 cm by 1.1 cm and the
epididymal cyst measures 3.3 mm by 2.0 mm by 4.2 mm, a little larger
than before. The testicle itself measures 3.48 cm by 2.25 cm by 3.38
cm, a little smaller than before, but maybe due to the measurements
being at a different angle.
|
||||
| July 26, 2007 (Thursday) |
I had a really bad time with the CT scan today.
First, even though I did my usual trick of drinking the oral contrast quickly without tasting it, I just couldn't finish the second bottle. It made me nauseous, and I felt sick to my stomach for the rest of the day. The nurse who was supposed to put in my IV for the IV contrast was quite inexperienced and had trouble getting the IV started. It was really painful, so I insisted he get a different nurse to do it. The replacement wasn't much better, but at least she got it in on the second try. But she didn't get a blood return when she flushed the IV, which is not a good sign. Later, when the tech hooked up the IV to the IV contrast infuser, it was painful the entire time the contrast was being injected. (The tech also spilled the optiray solution on my arm. This doesn't hurt, but the liquid feels a bit different and dries to a shiny sheen.) During the CT scan itself, I got a bad muscle cramp in my right arm from holding it over my head. My pinky and ring finger remained numb/tingly for most of the day. After the CT scan I went to my oncologist's office to have blood drawn for tumor markers and a CBC. The phlebotomist also had trouble drawing blood intially, because she tried using the same vein the inexperienced CT nurse had messed up. Her next attempt worked, but after each vial of blood she had to fish around a little to get it started again. My arm shook the entire time she was drawing blood. I then went to UPMC Montefiore to pick up the CD-ROMs from the dedicated scan of my pancreas. I must have looked like a human pincushion because the garage attendant waved me through instead of charging me for parking.
|
||||
| July 31, 2007 (Tuesday) |
I met with my oncologist today to review the semi-annual CT scan and
tumor marker tests and to discuss the pancreatic lesions. The CT scan
shows no sign of metastasis from the testicular cancer and the two
pancreatic lesions are unchanged in size. The Beta HCG and AFP tumor
markers are both normal at <2 mIU/mL (0-9 normal) and 2 ng/mL (0-6
normal). My blood glucose is mildly elevated at 118
mg/dL, indicating that diet and exercise are adequately controlling
it. Sodium was low normal (136 mmol/L vs range of 135-148) and
chloride was slightly low (95 mmol/L vs range of 96-109). ALT and AST
were up slightly from last time, but still normal, at 53 IU/L (normal
0-55) and 33 IU/L (normal 0-40).
My oncologist believes that the pancreatic lesions will turn out to be adenoma, a benign growth of glandular tissue. Unless the second biopsy on August 8 shows something different, he doesn't feel that surgery is indicated, as surgery would render me insulin dependent. He'd recommend adding surveillance of the pancreatic lesions to my testicular cancer surveillance. The two would mesh well, only requiring an occasional dedicated scan of the pancreas. The text of the CT scan report is as follows: CT CHEST, ABDOMEN AND PELVIS WITH CONTRAST A routine CT of the chest, abdomen and pelvis was performed, scanning from above the lung apices through the pubic symphysis after the administration of oral contrast and intravenous Optiray. INDICATION: Testicular cancer. COMPARISON: CT 12/21/2006, CT of the abdomen 6/21/2007, PET-CT 3/9/2007. FINDINGS CHEST: There is no pleural or pericardial effusion. The lung parencyma is clear. Subsegmental atelectasis at the left base. There is no thoracic lymphadenopathy. The bony thorax is normal. FINDINGS ABDOMEN: There is stable diffuse fatty infiltration of the liver. Status post cholecystectomy. The stomach, spleen, adrenals, kidneys are normal. The 2 hyperenhancing lesions in the tail of the pancreas are unchanged in size. No ascites, free air, or lymphadenopathy. FINDINGS PELVIS: The small bowel is normal. The appendix is not identified. The colon is normal. The ureters and bladder are normal. Change status post right inguinal orchiectomy are present. The visualized adbominopelvic vessels are normal. No free air, fluid or lymphadenopathy. The bony abdomen and pelvis are normal. Left iliac bone island is noted. IMPRESSION CHEST: 1. No evidence of metastatic disease. IMPRESSION ABDOMEN: 1. No evidence of metastatic disease. 2. Stable hyperenhancing pancreatic lesions. 3. Stable diffuse hepatic steatosis. IMPRESSION PELVIS: 1. No evidence of metastatic disease.
|
||||
| August 8, 2007 (Wednesday) |
I had a second endoscopic ultrasound and biopsy (EUS-FNA) today. The
original EUS-FNA (on May 14) did not yield a definitive diagnosis,
finding mostly acinar cells with two groups of mild to moderate
atypical ductal cells. (Subsequent blood tests ruled out acinar cell
carcinoma, as my amylase and lipase were normal.) The original EUS-FNA
also missed the 1.5 cm lesion in the body of the pancreas.
The purpose of the new biopsy was to:
Since I would be receiving general anesthesia, my wife had to drive. Allegheny General is pretty easy to get to from i275. (Allegheny General is one of only two hospitals in the region that can perform this kind of biopsy, and the only one that is in-network with my health insurance.) As we were getting ready to leave for the hospital we got a call from the GI lab, asking if we could come in early as they had had a cancellation. We left immediately, as this would let them start an hour earlier. When we arrived at the hospital I took a quick break at the bathroom. The bathrooms outside the GI lab smell like cinnamon. The prep was the same as last time, undressing just from the waist up. The nurse had to insert the IV in the back of my hand, as she had trouble finding a good vein elsewhere and didn't want to use a vein near my elbow. I do not like them to use the veins on the back of my hand, as my nerves run on top of those veins, so half the time they end up going through the nerve to reach the vein (hurts incredibly for hours). But this time she missed the nerve. After the doctor explained the plan and I signed the consent forms, they wheeled me into the procedure room and hooked up an EKG monitor and blood pressure monitor. The nurse had a bit of trouble hanging the IV bag; she kept on getting it tangled in some wires and put it on the wrong hook. Then she hooked up a nasal cannula to supply oxygen through my nose. Then we had to wait for 15 minutes because the anesthesiologist was delayed in radiology for an emergency. After he arrived and I signed the consent form, they had me turn on my left side and inserted a bite guard in my mouth. They also put a form-fitting backrest behind my back and had me scoot back against it. The last I remember is seeing 9:38 am on the monitors and a nurse removing my glasses. I woke up around 1:40 pm with a sore throat, tummy ache and a bit of a headache. The nurse had already removed the IV from my arm. The doctor said that he was unable to biopsy the body mass, as it was situated between two blood vessels. There would have been too great a risk of uncontrolled bleeding. But he was able to see it on the ultrasound, and it is definitely a mass. So he did two kinds of biopsies of the tail mass. One was the same fine needle aspiration as before, which obtains individual cells. The other used a larger needle to get an actual tissue sample (EUS-TCB), so the pathologist will be able to evaluate the structure of the mass. Because of the larger needle for the second biopsy, there was a greater risk of bleeding, so the doctor told me to drink only clear liquids today and ordered a CBC blood test for the next morning. I think the headache may have been caused by the supplemental oxygen getting dislodged or because the procedure may have been a little longer. (I worked for four hours after returning home, took a bath and went to bed early because of the headache.) The headache mostly cleared up by the next morning, and the sore throat by the weekend. It will take 1-2 weeks for the pathology/cytology reports to come back. The doctor will fax them to me, along with my other doctors. His preliminary report, based on what he saw on ultrasound, is recommending surgical intervention (a distal pancreatectomy). He says that there is a definite mass showing up in both locations on the ultrasound, and he doesn't think it is a benign adenoma. He says that he thinks the surgery would leave enough of the pancreas that I would not become an insulin dependent diabetic. The next morning we discovered that the doctor had written the wrong name on the prescription. The registrar kept on calling for "Rod". After a while she figured it out and called my name. She corrected the name on the prescription. The phlebotomist tried two times to hit a vein and had trouble both times, so she called a more experienced phlebotomist, who inserted the needle into the vein at the second site without problems.
|
||||
| August 28, 2007 (Tuesday) |
I saw my urologist today. He says that the ultrasound shows no
change. My urinalysis shows glucosuria, so the diabetes is starting to
cause sugar to leak into urine. It may be necessary for me to take
some oral medication to bring it under control, but he wants to
revisit it on my next appointment first.
The text of the ultrasound report is as follows: EXAMINATION PERFORMED: C-ULTRASOUND OF TESTES DATE: 07/24/07 10:46 HOURS CLINICAL HISTORY: Testicular microlithiasis; right orchiectomy for seminoma. COMPARISON: Multiple prior scrotal ultrasouns, the most recent dated 01/29/2007. TECHNIQUE: Sonography of the scrotum was performed. FINDINGS: There are stable postoperative changes from right orchiectomy; this is no abnormal tissue within the right testis fossa. The left testis measures 3.5 x 2.3 x 3.4 cm. No parenchymal mass is identified; there are unchanged multiple microcalcifications. The left epididymis is unchanged; there is an anechoic epididymal head cyst which measures 0.3 x 0.2 x 0.4 cm (previously it measured 0.2 x 0.2 x 0.2 cm). A small left hydrocele and varicocele are again noted. IMPRESSION: 1. STABLE POSOPERATIVE CHANGES FROM RIGHT ORCHIECTOMY. 2. NO LEFT TESTIS MASS WAS IDENTIFIED. 3. UNCHANGED MICROLITHIASIS AND SMALL LEFT HYDROCELE/VARICOCELE.
|
||||
| August 29, 2007 (Wednesday) |
I received a copy of the EGD Report and pathology report from my
second biopsy today.
The right side of the EGD Report was truncated by the sender's fax machine, but it was mostly readable. The surgeon is recommending surgical intervention (distal pancreatectomy). The pathology report was again inconclusive, but the pathologist is leaning toward a diagnosis of Islet cell tumor (neuroendocrine tumor of the pancreas). The text of the pathology report is as follows: CYTOLOGY (NON-GYN) REPORT Specimen(s) Received A: TAIL OF PANCREAS, FINE NEEDLE ASPIRATION, CYTOLOGY AND CELL BLOCK Addendum Diagnosis FINAL PANCREAS, TAIL LESION, FINE NEEDLE ASPIRATION, CYTOLOGY AND CELL BLOCK 1. SMALL GROUPS OF ENDOCRINE CELLS (SEE NOTE) Addendum Comment Immunostains were performed on the cell block for synaptophysin, chromogranin and NSE. These stains are negative, however, the amount of cells present in the cell block is very limited. Based on morphology, it is favored that the small groups represent endocrine cells, raising the possibility of an Islet cell tumor. However, a definitive diagnosis cannot be rendered due to limited material and cell distortion. Diagnosis PRELIMINARY PANCREAS, TAIL LESION, FINE NEEDLE ASPIRATION, CYTOLOGY AND CELL BLOCK: 1. SMALL EPITHELIAL GROUPS: ENDOCRINE VERSUS ACINAR 2. FINAL DIAGNOSIS PENDING IMMUNOSTAINS So at this point the options are:
|
||||
| October 26, 2007 (Friday) |
I received the cytology report from the second opinion on my second
biopsy. The text of the report is as follows:
FINAL DIAGNOSIS: FNA tail of pancreas -- seventeen outside slides labeled N07-1823: UNSATISFACTORY. NON-DIAGNOSTIC SPECIMEN. GASTROINTESTINAL CELLS AND OCCASIONAL SMALL GROUPS OF POSSIBLE ENDOCRINE CELLS PRESENT, BUT SPECIMEN IS INSUFFICIENT FOR DIAGNOSIS.
|
||||
| November 19, 2007 (Monday) |
I met with my gastroenterologist today. He was quite
emphatic in saying that I should go forward with the
surgery. He said that while there is not a definitive
diagnosis, there is enough there that is suspicious for
cancer that I should have it removed. He said that
another biopsy would not provide any additional information.
He added that if I insist on waiting to obtain a definitive
diagnosis, by then it will have metastasized and there'll
be nothing I can do about it. He does not recommend
removing just the tail mass, as there is no possibility
for a rush pathology during the surgery.
My next step is to meet with my oncologist to see what he says, since he's been opposed to surgery. I feel like I'm being forced to make a decision between two difficult outcomes without sufficient information to make a rational choice. On the one hand, if it is islet cell tumor (neuroendocrine tumor of the pancreas), the only effective cure is surgical resection before it metastasizes. My understanding is that such tumors only start to achieve malignant potential when they reach about 2 cm in size. On the other hand, surgery would likely render me an insulin-dependent diabetic and maybe also needing daily pancreatic enzymes. I would also lose the spleen. I don't want to risk this if the two masses are benign, as that could have serious implications for my quality of life. Clearly, if this is cancer it's been indolent since 2003, since both masses were present in my original staging CT scan from the testicular cancer and are unchanged in size. So one might argue that if they haven't done anything in four years, they probably aren't cancer. But that doesn't necessarily mean anything, since islet cell tumor is a very slow-growing form of cancer that frequently goes indolent and very little is known about the natural history of this type of cancer. (See Population-Based Study of Islet Cell Carcinoma.) I'm a quantitative guy, and all I've got is vague qualitative information and some opinions that are not really supported by evidence or experience. When I don't have enough information to make a decision, my natural inclination is to try to obtain more information. But I'm getting the sense that further biopsies will not be any more definitive than the first two. Plus, it is difficult to prove a negative, so if this is benign a biopsy wouldn't necessarily help. So what do we know?
The odds of having simultaneous testicular cancer and neuroendocrine tumor of the pancreas are astronomical. I found no prior cases in the medical literature. When I asked one of my doctors what percentage of cases similar to mine turned out to be benign after surgery, his answer was that there were no similar cases. At this point my gut instinct (pun intended) is that the masses might be benign, but neither possibility can be ruled out, and I probably can't risk the possibility of it being cancer. But I'm also very concerned about needing insulin and pancreatic enzymes. I've read that pancreatic enzymes can have side effects of abdominal cramps, bloating, gas, belching, indigestion, diarrhea and weight loss. They can also lead to the development of food allergies. My current thinking is that maybe I should obtain a biopsy elsewhere (e.g., at Johns Hopkins or Sloan Kettering). I've asked my doctors about surveillance protocols, and they've suggested quarterly dedicated scans of the pancreas, but I haven't seen any data on the effectiveness of such a protocol. I'm also thinking of paying a medical research firm to provide a comprehensive review.
|
||||
| November 20, 2007 (Tuesday) |
The surgeon at West Penn Hospital who originally recommended against
surgery is again recommending against surgery. He says that with no
size change in four years, no symptoms, staining negative for NSE,
synaptophysin, chromogranin, and nothing in the biopsy (the atypical
ductal cells in the first biopsy are probably due to the
pancreatitis), he believes the two masses to be benign (not malignant).
He also mentioned that the UPMC surgeon who is recommending surgery is young and has a 22% fistula rate with the laparoscopic procedures, which is considered high, and an average 18-day hospital stay. He said that the easiest thing for any surgeon to do is to operate, but he would not recommend pursuing this any further. He will consult with Dr. Jeffrey Norton at Stanford to confirm this approach. Dr. Norton is the national expert on Islet cell tumors. My feeling at this point is that unless Dr. Norton recommends surgery, I will pursue surveillance. As far as surveillance is concerned, he would suggest a pancreatic protocol CT scan (dedicated scan of the pancreas) every six months, along with markers. He will talk to my oncologist about integrating this into my surveillance protocol for testicular cancer (CT scan chest/abdomen/pelvis every six months).
|
||||
| November 20, 2007 (Tuesday) |
The letter from my gastroenterologist to my oncologist is a bit milder
than his emphatic statements in person. The last paragraph of the
letter is excerpted below.
I did explain to Mark that I wasn't sure that I could offer much to add any insight into the nature of his cyst. It's been there for four years. It does apear that there is suspicion for malignancy or at least for a precancerous change and, based on that in a young male, I thought it was enough to consider getting surgical resection. Of course, there is a risk that this could be completely benign and that he may suffer a complication from his surgery but the other risk would be that we can continue to monitor this and it becomes frankly malignant and then untreatable at that time. I told him unfortunately I was not sure that there was anything else that would help elucidate this and that he would have to make his informed decision based on the information at hand. My feeling is that he probably should undergo the surgery despite the attendant risk because I think that the risk of waiting until a potentially precancerous lesion becomes malignant would have a devastating impact and may ultimately lead to an incurable state. I did tell him, however, that there is also a flip side that there is a small chance that it would be completely benign and unfortunately having this resection would leave him possibly needing chronic pancreatic enzyme replacement; perhaps even insulin. I told him he probably should discuss this further with his surgeons and his oncologist and make his informed decision. I didn't think that there was much else I could offer to help clarify the nature of these cysts except to add that clearly both fine needle aspirations seem suspicious.
|
||||
| December 17, 2007 (Monday) |
Early this morning I woke up choking on my own vomit and had
difficulty breathing for a minute. I don't think this was connected to
anything, just some acid reflux that got aspirated. I tilted the bed a
little and went back to sleep on my left side after eating a few
Tums. My throat hurt for the rest of the day.
If it happens again, I'll mention it to my doctor.
|
||||
| December 20, 2007 (Thursday) |
I had my semi-annual CT scan today.
Traffic was horrible. I tried taking the 31st street bridge, which had reopened recently, but the traffic on Route 28 to the bridge crawled. I got a bit annoyed at the car in front of me. It was a Humane Society minivan, and the driver was not at all paying attention to the road. It looked like he was writing something. He weaved a little bit, and stopped suddenly for no apparent reason. There was nobody in the waiting room at registration, so I was seen right away. This time I brought a printout of all my previous imaging studies, which also saved some time in completing the paperwork. Today's nurse was experienced and able to insert the IV on the first try. I drank the first container of oral contrast in the space of a few seconds. I was trying to avoid tasting it. The second container took longer, and I wasn't able to finish the last centimeter as it made me nauseous. The CT was the older machine, not the new 64-slice machine, so it took a little longer. But it was uneventful, with the usual feeling of heat at the back of the throat and base of the tush. I then drove to my oncologist's office to have blood drawn for tumor markers. The phlebotomist, Mandi, had a different hair color and is five months pregnant. She also inserted the needle into a vein on the first try, but it slipped in further when she changed tubes, probably collapsing the vein. She checked whether she had enough blood for the tests, and used a finger stick for the CBC. I had loud bowel noises and everything else that accompanies consumption and elimination of oral contrast for the rest of the day. I also seem to have caught a bad cold at the hospital. The best way to get sick is to visit a hospital, because there are a lot of sick people there.
|
||||
| January 8, 2008 (Tuesday) |
I met with my oncologist today to discuss my recent CT scan and tumor
markers and to discuss the two pancreatic masses.
My tumor markers are all normal. Beta HCG is less than 2 mIU/mL (0-9 is normal), AFP is 2 ng/mL (0-6 is normal), and CA 19-9 is 4 U/mL (0-35 is normal). My oncologist added CA 19-9 because of the pancreas. He also ran a comprehensive metabollic panel and CBC as he usually does. AST (SGOT) and ALT (SGPT) were both slightly elevated, with AST at 43 IU/L (0-40 is normal) and ALT at 59 IU/L (0-55 is normal). Serum sodium and chloride are just slightly below the low end of normal. Blood glucose is 199 mg/dL, twice normal, a sign that my diabetes is out of control. I will need to lose some weight and exercise more. Everything else was normal. The CT scan report was also fine. The text of the report is as follows: CT CHEST, ABDOMEN AND PELVIS WITH CONTRAST DEC 20, 2007 1:23:00 PM A routine CT of the chest, abdomen and pelvis was performed, scanning from above the lung apices through the pubic symphysis after the administration of oral contrast and intravenous Optiray. INDICATION: Testicular cancer COMPARISON: CT of the chest abdomen and pelvis dated 7/26/2007. FINDINGS CHEST: There is no pleural or pericardial effusion. There is minimal left basilar subsegmental atelectasis. The lung parenchyma is otherwise clear. There is no thoracic lymphadenopathy. The bony thorax is normal. FINDINGS ABDOMEN: The liver demonstrates table diffuse fatty infiltration and surgical clips are present in the gallbladder fossa from prior cholecystectomy. The stomach, splee, adrenals and kidneys are normal. Previously noted hyperdense lesion in the distal pancreatic tail in unchanged from multiple prior examinations. The more proximal hyperdense pancreatic lesion is not seen on today's examination. No ascites, free air or lymphadenopathy. FINDINGS PELVIS: The small bowel is normal. The appendix is not identified. The colon is normal. The ureters and bladder are normal. The visualized abdominopelvic vessels are normal. No free air, fluid or lymphadenopathy. Again noted is a small bone island in the left iliac bone, unchanged. IMPRESSION CHEST: 1. No evidence of metastatic disease. IMPRESSION ABDOMEN: 1. No evidence of metastatic disease. 2. Stable appearance of the hepatic steatosis. 3. Stable hyperdense lesion in the distal pancreatic tail. IMPRESSION PELVIS: 1. No evidence of metastatic disease. My oncologist believes the pancreatic masses to be benign and recommends against surgery. I have decided to not have surgery for the following reasons:
Instead, I will undergo surveillance consisting of a dedicated CT scan of the pancreas every six months. This will look for signs of growth. Eventually it will drop to annual scans. It will be integrated into my regular surveillance for my original cancer. My oncologist will also order any tumor markers permitted by my insurance.
|
||||
| January 25, 2008 (Friday) |
I had my semi-annual ultrasound today. I glanced at the images and
didn't see any problems. I also had blood drawn for PSA and
testosterone tests.
|
||||
| February 26, 2008 (Tuesday) |
I met with my urologist today for the semi-annual clinical testicular
exam and to review the results from my PSA and testosterone tests. He
threw in a prostate exam since I hadn't had one in a while. The
prostate was normal. My PSA was 0.2 ng/ML using the Bayer
chemiluminescence method (normal 0-4). My ultrasounds were normal.
My urinalysis showed glucosuria, a sign that my diabetes is not under control. He recommended following up with my PCP. My total testosterone was 157 ng/dL (normal 250-1100), down from 193 in February 2007 and 255 in January 2006. My free testosterone was 3.14% (49.3 pg/mL), up from 2.55% (49.2 pg/mL) in February 2007 and 2.36% (60.1 pg/mL) in January 2006. Normal is 35 to 155 pg/mL and 1.5% to 2.2%. The percentages are increasing because the total testosterone is decreasing. So I am again clearly testosterone deficient, although I'm generally asymptomatic. I have been experiencing a bit greater difficulty concentrating and slight short-term memory loss, but those are not severe and not specific to testosterone deficiency. I have not been experiencing any of the more specific symptoms of testosterone deficiency, such as night sweats, hot flashes or irritability. There has been some diminished libido. My urologist has ordered a bone density test to establish a baseline, since low testosterone puts me at risk of osteoporosis. He has also ordered tests for LH, FSH, prolactin and SHBG. If any of those are abnormal, he'll prescribe testosterone replacement therapy (TRT). Otherwise he's leaving the decision to use TRT up to me.
|
||||
| February 28, 2008 (Thursday) |
I had my bone density scan (DEXA) today at UPMC Passavant
Cranberry. It was quick and straightforward. I had to remove all metal
from my pockets (watch, cell phone, digital camera, pen, wallet, keys,
pocket knife, change) and my belt. The platform was similar to that of
a CT scan, but in this case the scanner moved instead of the
platform. First the technician put my legs up on a platform,
effectively putting me into a seated position but lying on my
back. This was to scan my spine. Then she removed the support from my
legs and stretched them out, velcroing my feet to a triangle that
turned my legs inward, toes pointing to each other. This was a little
uncomfortable, but it wasn't for long. This was for scanning my hips.
I also had my blood tests (FSH, LH, prolactin and SHBG). This took a lot longer than the bone scan. First, the receptionist was unable to photocopy my card because the photocopier was out of paper and she had to ask someone where to get some paper. When nobody knew, she found another photocopier to use. Then the person at registration sat doing nothing for a while before calling me over. I think she forgot about the patients in the waiting room, because she was doing nothing. Then at the lab, the phlebotomist took my paperwork and then had me wait for a while. It was taking so long that the person ahead of me got annoyed, asked for his paperwork and left. I think that prodded her to speed up a bit. Other than that, she was a good phlebotomist, hitting the vein correctly on the first try.
|
||||
| March 12, 2008 (Wednesday) |
I received the results of my blood tests and bone scan today.
FSH was 4.0 mIU/mL (1.0 to 18.0 normal), LH was 3.1 mIU/mL (2.0 to 9.0 normal) and Prolactin was 3.0 ng/mL (1.0 to 20.0 normal), all normal. SHBG was below normal at 8 NMOL/L (9 to 45 normal). It is likely that the low SHBG is the cause of normal free testosterone despite deficient levesl of total testosterone. It is likely that the SHBG is low because of my diabetes. If I were to lose weight the SHBG might increase, which would result in lower free testosterone and I might then become symptomatic of testosterone deficiency. Bone density at the left hip was normal, but bone density in the spinal cord (vertebrae L1 through L4) was in the osteopenic range. This is likely due to testosterone deficiency. I will need to follow up with my PCP regarding the osteopenia. Most likely I will need to take calcium and vitamin D supplements such as Viactiv. I will also likely need to go on testosterone replacement therapy. As a precaution I will ask my doctor about checking my estradiol (E2) levels and also checking for hypothyroidism. The text of the bone scan report was as follows: EXAM DATE: 02/28/08 C-BONE DENSITY CLINICAL HISTORY: Hypogonadism secondary to orchiectomy. FINDINGS: Bone densitrometry evaluation is performed utilizing Hologic QDR 4500 technique. The following results were obtained and represent mean values for each region. Bone density, left hip: 0.916 gm/cm2 T score: -0.2 Standard deviations IMPRESSION: WHO diagnostic guidelines; normal bone density. Bone density, L1 through L4 anterior: 0.906 gm/cm2 T score: -1.3 Standard deviations IMPRESSION: WHO diagnostic guidelines; osteopenia. WHO DIAGNOSTIC GUIDELINES Normal - T score > (-)1.0. Osteopenia - T score - (-)1.0 to (-)2.5. Osteoporosis - T score < (-)2.5. Severe osteoporosis - T score < (-)2.5 + fracture. T-score - comparison of patient's current bone mineral density to mean for age at which peak bone density is achieved.
|
||||
| July 21, 2008 (Monday) |
I had my semi-annual CT scan and tumor markers today.
The CT scan
combined the imaging study of chest/abdomen/pelvis with a pancreatic
protocol scan of the pancreas. It took a little longer as a result, and
they added some shielding of the chest area. It took two CD-ROMs to hold
all the images.
The bench in which they store the gowns has a new wooden seat. The old one had a laminate seat. The "one in front and one in back" sign is unchanged. After I changed into the gowns the receptionist gave me the two bottles of oral contrast to drink. I wasn't able to finish both bottles of oral contrast as I wasn't feeling well, leaving an inch or so in one of the bottles. The contrast solution was the same as in previous CT scans, but tasted worse this time for some unknown reason. I also got the "topped-off to the gills" feeling a lot quicker even though I was using the same "drink quickly to avoid tasting it" technique. After I finished most of the oral contrast a nurse called me over to a room just off of the waiting room to have my IVs inserted. They have the IVs inserted there, instead of in the CT scan room, to make more efficient use of the CT scan equipment (e.g., pipelining the process). They're using tegaderm now to cover the IVs instead of tape. It's a little easier to remove. My IV was inserted by a trainee nurse who had trouble on the first attempt and tried unsuccessfully to recapture the vein by fishing around with the needle. After causing me the requisite amount of pain she asked the supervising nurse to take over rather than turn me into a pincushion. The supervising nurse found the vein on her first attempt. So all in all, it wasn't too bad. In addition to the usual blood tests my oncologist ordered a 5HIAA urinalysis (a pancreatic tumor marker), which requires 24 hour collection. I can't start it today because of the oral and iv contrast from the CT scan, so I'll start it tomorrow and take off an hour plus lunch break on Wednesday to deliver it to my oncologist's office. I glanced at the slides and didn't see anything obvious. I won't know for certain until I meet with my oncologist to review the radiologist's report. Since this represents the 5-year mark, I expect that my oncologist will reduce the frequency of my follow-up from semi-annual to annual.
|
||||
| July 22, 2008 (Tuesday) |
I filled the 3000 ml jug with urine today. As per the instructions, I
skipped the first urine of the day after waking in the morning and
started the collection with the next. I had no trouble filling the jug
throughout the day because I was drinking a lot because I felt
thirsty. I stopped filling the jug in the evening because it was
completely full. I felt a little weird storing urine in the refrigerator.
|
||||
| July 23, 2008 (Wednesday) |
I drove to my oncologist's office to deliver the jug of urine. I
carefully propped up the jug with towels and drove carefully because
the last thing I wanted was to have to clean up spilled urine from my
car.
I noticed that the state police were out stopping cars for speeding. I wasn't stopped, but I imagined explaining to the police officer why I had a large jug of urine in the back of my car.
|
||||
| July 28, 2008 (Monday) |
I saw my oncologist today for my semi-annual exam and to review the
results of my CT scan and tumor markers. Everything was normal and
stable. He considers me cured of the original testicular cancer and
believes the pancreatic masses to be benign adenomas. He recommends
that I see an endocrinologist for management of my diabetes,
testosterone deficiency and osteopenia as he does not feel they can be
adequately managed by a non-specialist.
Tumor markers for testicular cancer were normal, with AFP at 2 ng/mL (0-6 is normal) and beta HCG negative (< 5 mIU/mL). Tumor markers for the pancreas were normal, with CA-19-9 at 13 U/mL (0-35 is normal), Chromogranin A at 2 nmol/L (0-5 is normal), and 5-HIAA 24-hour urine at 2.1 mg/24 hr (0-8 normal) and 0.7 mg/L. WBC were normal at 7.2 (7.0 +/- 3.0), RBC at 5.17 (5.4 +/- 0.7), HGB at 14.8 (16.0 +/- 2.0), HCT at 45.3 (47 +/- 5), MCV at 87.5 (87 +/- 7), MCH at 28.6 (30.2 +/- 3.6), MCHC at 32.7 (33.9 +/- 2.4), and platelets at 212 (150-400). The text of the CT scan report was as follows: INDICATION: Testicular cancer, pancreatic mass IMPRESSION: Chest: No metastatic disease Abdomen: 1. Stable 1 cm hypervascular mass in the pancreatic tail 2. No metastatic disease 3. Fatty infiltration of the liver Pelvis: No metastatic disease Triphasic imaging of the pancreas was performed with oral and IV contrast. Enhanced images were also obtained of the chest and pelvis. Compared to 12/20/2007. No nodules in the lungs. No pleural effusion. No enlarged intrathoracic lymph nodes. Mild dependent atelectasis in the lower lobes bilaterally. Diffusely fatty infiltration of the liver. No hepatic mass. Cholecystectomy. Spleen is normal. 1 cm hypervascular mass in the pancreatic tail is stable. No new or additional lesion is present the pancreas. Adrenal glands and kidneys appear normal. No enlarged retroperitoneal or mesenteric lymph nodes. Small bowel and colon appear normal. No pelvic lymphadenopathy or free fluid.
|
||||
| August 8, 2008 (Friday) |
I received copies of blood tests ordered by my primary care
physician. The tests demonstrate that my diabetes is out of control,
with fasting blood glucose at 417 mg/dL (normal 75-100) and Hemoglobin
A1C at 14.7% (normal 4.8-6.0). Also, the urinalysis shows glucosuria
(glucose > 1000 mg/dL, ketone 15 mg/dL).
Other abnormal test results include NA at 131 (normal 135-145), CL at 93 (normal 95-109), high cholesterol at 247 (normal 10-199), high triglycerides at 439 (normal 10-199). HDL was normal at 39 and LDL normal at 120. SGOT (AST) low at 14 (normal 15-40). Normal kidney function. The albumin/creatinine ratio, however is high at 31.6 (normal 0-20).
|
||||
| August 26, 2008 (Tuesday) |
No signs of any problems (other than glucosuria) at my semi-annual
urologist appointment. Since this is the 5-year mark, we will be
switching to annual exams from this point onward.
It is curious that the testicle is 1 cm or so longer in the longest dimension. But there is no sign of any focal masses, so this is not of concern. Most likely this was due to a different angle of measurement. The text of the ultrasound report was as follows: EXAMINATION PERFORMED: C-ULTRASOUND OF TESTES DATE: 07/30/08 12:53 HOURS CLINICAL HISTORY: The patient is a 41-year-old male with history of right orchiectomy for a seminoma. TECHNIQUE: High-resolution gray scale ultrasound imaging of the scrotum was performed. FINDINGS: The left testis measures 4.6cm x 2.4cm x 3.4cm. Multiple punctate calcifications are seen throughout the testes which are likely secondary to testicular microlithiasis. No definite dominant mass is identified. Normal arterial flow is demonstrated within the testes. The epididymis appears unremarkable. Multiple tortuous vascular channels are seen above the testes which increase flow on Valsalva which may represent presence of a small varicocele. A small amount of fluid is seen within the left scrotum. IMPRESSION: 1. LEFT TESTICULAR MICROLITHIASIS IS SEEN. NO DEFINITE TESTICULAR MASS IS IDENTIFIED. 2. THE RIGHT TESTIS IS SURGICALLY ABSENT. 3. PROMINENT VASCULAR CHANNELS SEEN ABOVE THE LEFT TESTIS WHICH INCREASE IN SIZE ON VALSALVA WHICH MAY REPRESENT PRESENCE OF A SMALL VARICOCELE.
|
||||
| October 7, 2008 (Tuesday) |
I saw an endocrinologist at Allegheny General Hospital to address my
diabetes and testosterone deficiency. My blood glucose levels have
been above 400 for several months and have not responded to diet and
exercise (lost 35 pounds) nor medication (glucophage). The
endocrinologist believes I am suffering from insulin insufficiency (as
opposed to insulin intolerance) stemming from the cisplatin induced
pancreatitis I had five years ago. Apparently it can take time for the
damage to become evident. He also believes that the two masses in the
pancreas are probably due to inflammatory changes from the
pancreatitis. (Of course, the two masses were present on the staging
CT scan, which predates the pancreatitis, so that hypothesis probably
isn't correct.)
His plan is to first address the diabetes and then revisit the testosterone deficiency and osteopenia. He says that diabetes can inhibit testosterone production so some of the deficiency may be due to that. (He pointed at the normal FSH and LH as a potential indication for it to not be primary hypogonadism.) Likewise diabetes can contribute to osteopenia. It will also be easier to diagnose when the blood glucose levels have normalized. He is ordering a total of 33 fasting blood tests and a 24-hour urine collection. The blood tests include gonadal function (total testosterone, free testosterone, bioavailable testosterone, SHBG, estradiol, FSH, LH), pituitary function (IGF-1, prolactin), calcium (calcium, albumin, phosphorus, magnesium, 25-hydroxy vitamin D, intact PTH), diabetes (Hemoglobin A1C, antigad 65 antibody, C-Peptide), hematology (CBC with differential, platelets), general chemistory (comprehensive metabolic panel, serium iron, ferritin, tibic, vitamin B12, folate), lipids (total cholesterol, hdl, ldl, tg, vap, total cpk), thyroid function (t4 total, t3 uptake, tsh high sensitivity, antimicrosomal antibodies, thyroglobulin antibody). The urinalysis includes protein, creatinine clearance and microalbumin. He is prescribing intensive insulin with two types of insulin, Lantos and Novolog, one for a baseline longer-lasting insulin level and the other before meals. I have an appointment with a nurse to undergo diabetes education again.
|
||||
| October 8, 2008 (Wednesday) |
This morning I had blood drawn for the 33 blood tests. The
phlebotomist hit a good vein on the first try, and then proceeded to
exsanguinate me, filling 17 vials with blood. I have five days to
collect and return a 24-hour urine or they'll have to draw blood again
(but only one vial). [On October 17-18, 2008 the lab billed my
insurance a total of $5,147,25 and was paid at UCR a total of
$4,375.19.]
Between the 14 hour fast and the blood draw I was a little light-headed, so I stopped by a pharmacy to fill the insulin prescription and get some munchies.
|
||||
| October 22, 2008 (Wednesday) |
I had my diabetes education today. The intensive insulin therapy
includes Lantos (slow acting insulin) and Novolog (fast acting
insulin). I will be taking 20 units of the Lantos once a day to
establish baseline insulin levels and the Novolog before meals. The
number of units of Novolog will depend on my blood glucose levels and
the number of carbohydrates. 10 grams of carbohydrates corresponds to
one unit of insulin, and every 50 ng/dL of blood glucose above my
target (100 ng/dL) to one unit of insulin. This yields the following
formula:
# units of insulin =
grams of carbohydrates / 10 +
(blood glucose - 100) / 50.
I will be taking the Lantos at night. If my blood sugar is too low in the morning, I will start taking it in the morning instead. My blood glucose targets are 100 ng/dL before meals and 140 ng/dL two hours post-prandial. I have two insulin pens, one for each type of insulin. The insulin needs to be refrigerated until it is installed in the pens. Once installed in the pens, the insulin does not need to be refrigerated and is good for 30 days.
|
||||
| October 23, 2008 (Thursday) |
My first day of insulin was ok. Four injections a day, plus more
frequent monitoring of blood glucose. I had a little more energy, but also
more fatigue and somewhat irritable. Some abdominal upset (probably
not related to my giving
myself the four injections in my abdomen). My blood glucose did come
down a bit, to around 300. I probably need to increase the insulin
dosage.
|
||||
| October 24, 2008 (Friday) |
I received a copy of the test results from my October 8, 2008 blood
tests and urinalysis.
Hematocrit was a little low at 40.3% (reference range 42.0 to 52.0), possibly a sign of dehydration from the diabetes. The rest of the CBC was within the normal range. Sodium (NA) was a little low at 132 mEq/L (reference range 135-145). Fasting blood glucose was high at 394 mg/dL (normal 75-100). Note that this was after a 14-hour fast. Hemoglobin A1C was high at 15.1%. C-Peptide was 1.4 NG/ML (normal 0.8 - 3.1). Somatomedin-C (insulin-like growth factor 1) was low at 74 ng/mL (normal 86-220). Cholesterol was high at 299 mg/dL (normal 10-199), probably a side effect of the high blood glucose. Triglycerides were 835 (normal 10-199) and HDL was 36 mg/dL. LDL was not calculated because of the high triglyceride levels; instead a direct measurement was ordered, yielding 100 mg/dL (0-129 is normal). CK (Creatine phosphokinase) was low at 13 U/L (24-210 normal). Bilirubin (0.7 mg/dL), protein (7.6 g/dL), ALB (3.5 g/dL), AST (19 U/L) and ALT (42 U/L) were all normal. BUN/CREAT ratio was 13. Estimated GFR was greater than 60 mL/min/1.73m^2 indicating normal kidney function. Magnesium (1.9 mg/dL), Iron (86 ug/dL), total iron binding capacity (267 ug/dL), vitamin B12 (395 pg/mL) and ferritin (296 ng/mL) were all normal. Folate was high at > 24 ng/mL. Calcium (8.9 mg/dL) was normal. Vitamin D 25-Hydroxy was normal at 39 ng/mL (normal 20-100) as was Vitamin D 250HD3 at 39. Vitamin D 25OHD2 was <4 ng/mL. Vitamin D levels are therefore sufficient. T4 (8.6 ug/dL), T3 (109 ng/dL), TSH High Sensitivity (1.1 mU/L) and Intact parathyroid hormone (24.2 pg/mL) were all normal. Thyroid Peroxidase AB (TPO) was < 10.0 IU/ML (normal < 35) and Thyroglobulin Antibody was < 20.0 IU/ML (normal < 20). The urinalysis showed creatinine of 0.9 mg/dL (normal 0.8-1.3) and urine volume 5900 mL. Total protein was not calculated because the levels were below 6 mg/dL. Creatinine clearance was 72 mL/min (70-130 normal). Urine creatinine was 1.0 gm/24 hours (normal 0.6-2.5). Microalbumin was 12.0 mcg/min (normal 0.0-20.0). With regard to the testosterone deficiency, LH (5.5 mIU/mL, normal 2.0-9.0), FSH (4.9 mIU/mL, normal 1.0-18.0), Prolactin (4.0 ng/mL, normal 1.0-20.0) and Estradiol (27 PG/ML, normal <= 29) were all normal. SHBG was low at 6 NMOL/L (normal 9-45). Testosterone levels as measured by Quest Diagnostics were as follows: Total Testosterone was low at 226 ng/dL (normal 250-1100), Free Testosterone was normal at 71.2 pg/mL (normal 35-155) and Free Testosterone Percentage was high at 3.15% (normal 1.5% to 2.2%). A second set of tests were performed by a reference laboratory: Total Testosterone was low at 195 ng/dL (normal 250-1100), Free Testosterone was normal at 70.7 pg/mL (normal 46-224), Bioavailable Testosterone was normal at 126.9 ng/dL (normal 110-575) and Albumin was normal at 3.9 g/dL (normal 3.6-5.1) The normal free testosterone with normal FSH and LH but low SHBG suggests that the testosterone deficiency is not symptomatic because of the diabetes. As the diabetes gets under control the testosterone deficiency will likely become symptomatic.
|
||||
| November 25, 2008 (Tuesday) |
I had blood drawn in advance of my follow-up appointment with the
endocrinologist on December 2, 2008. He ordered the same set of tests,
including 24 hour urine collection and 17 vials of blood. I was
initially a little concerned because the nurse had mailed me a
photocopy of the 10/7/08 prescription ordering the tests instead of a
new prescription, but she said that Dr. Gordon always orders a lot of
tests.
I had a bad headache after the exsanguination and took a nap for the rest of the morning. It helps a little.
|
||||
| December 3, 2008 (Tuesday) |
I met with my endocrinologist. He increased my nightly dose of Lantos
insulin to 40 units and changed the formula for before-meal Novolog insulin to
1 unit for every 30 mg/dL of blood glucose over the target of 100
mg/dL, plus 1 unit for every 7 grams of carbohydrates. Previously I
was at 30 units (up from 20 units) of Lantos a night and 1 unit of
Novolog for every 50 mg/dL of blood glucose over the target of 100
mg/dL, plus 1 unit for every 10 grams of carbohydrates. He also gave
me a shot of vitamin B12 because I was a bit low and prescribed a
highly bioavailable version of B12 for me to take daily.
I also got my latest blood tests back. Key test results and tests that were outside the normal range include:
Several additional tests are still pending. My endocrinologist expects the cholesterol to normalize with further improvements in blood glucose control. We will wait until my next set of tests to determine what to do about the testosterone deficiency. It is possible that getting the diabetes under control may lead to improvements in testosterone production. I am experiencing night sweats, but I can handle it for another 3 months.
|
||||
| February 26, 2009 (Thursday) |
During the landing on a plane flight yesterday, my left ear did not
equalize air pressure correctly. It was a painful descent and I lost
hearing in the ear. I also had a nosebleed. My PCP took one look at
the ear and said "oh my". The ear drum was completely inflamed. I am
on antibiotics, anti-inflammatory drugs, nasal corticosteroids and
sudafed, and may need to see an ENT on Monday if there is insufficient
improvement over the weekend.
|
||||
| March 12, 2009 (Thursday) |
I saw my endocrinologist again today for my quarterly appointment. My
blood glucose continues to be volatile and I continue to gain
weight. My morning (fasting) blood glucose has been averaging 160
mg/dL (lab tests measured it at 139 mg/dL), an indication that the
Lantos dose is too low, so the doctor increased the dose to 50 units,
up from 40.
Blood test results were as follows: Cholesterol was high at 209 mg/dL (normal 10-199), with triglycerides at 91 mg/dL (normal 10-199), HDL at 41 mg/dL (moderate risk factor for chronic heart disease) and LDL calculated borderline high at 150 mg/dL (normal 0-129). AST was high at 42 U/L (normal 10-40) and ALT was high at 83 U/L (normal 25-75). Folate was high at >24.0 ng/mL (normal 5.3-24.0) an vitamin B12 was high at >2000pg/mL (normal 200-1000). Hemoglobin A1C was slightly high at 6.4% (normal 4.8-6.0), a significant improvement from 11.1%. Hemoglobin A1C is a long-term measure of diabetes control. Total testosterone was deficient at 223 ng/dL (normal 250-1100), but free testosterone was low normal at 62.5 pg/mL (normal 46.0-224.0) and bioavailable testosterone was low normal at 120.3 ng/dL (normal 110.0-575.0), probably because the SHBG was low normal at 10 NMOL/L (normal 9-45). So I am asymptomatic of testosterone deficiency despite the below normal total testosterone because the bioavailable testosterone is within the normal range. Most likely there is an interaction between the diabetes and the SHBG that is suppressing SHBG and permitting a normal bioavailable testosterone despite the below normal total testosterone. As the diabetes gets under control, SHBG will likely increase, causing bioavailable testosterone to decrease and I will likely become symptomatic of testosterone deficiency.
|
||||
| April 21, 2009 (Tuesday) |
The US Patent and Trademark Office has granted me a patent on my
technology for optimizing cancer follow-up surveillance
schedules. US Patent Number 7,523,043, Method for Minimizing the Cost
of Post Treatment Follow-up and Diagnostic Tests, issued today.
|
||||
|
|
|||||
|
|
|||||
|
|
Causes | Checklist | Costs | Cancer Jokes | Cancer Scholarships | Sites